Toolkit for developing a multisectoral action plan for NCDs
1. Conducting a comprehensive assessment
Noncommunicable diseases (NCDs) are the leading cause of death globally, killing more people each year than all other causes combined. Contrary to common perceptions, available data show that nearly 80% of NCD-related deaths occur in low- and middle-income countries. Moreover, recent decades have witnessed a steady increase in such deaths, with vulnerable population groups often worst affected, and yet many of the dire human and social consequences could be prevented by implementing costeffective and feasible interventions
The Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases (2011) (1) recognizes the scale of the NCD crisis and the urgent need for action. The Global action plan for the prevention and control of NCDs 2013–2020 (2), recently extended to 2030, provides a vision and a road map to scale up action for the prevention and control of NCDs.
The global epidemic of NCDs is widely acknowledged as a major challenge to development in the 21st century and is a significant threat to achieving the United Nations Sustainable Development Goals. In addition, globally, the main NCDs represent the greatest cause of death in people aged under 70 years, imposing years of disability on those affected and their families. The Global status report on noncommunicable diseases 2014 (3) highlights the need to intensify national multisectoral action to meet the global targets that governments have agreed upon and to protect people from cardiovascular diseases, cancers, diabetes and chronic respiratory diseases.
Countries, including some that are low income, are showing that it is feasible to make progress and reduce premature deaths from NCDs. But that progress, particularly in low- and middle-income countries, is insufficient and uneven. The global status report of 2014 reveals a distressing gap in our ability to achieve Sustainable Development Goal target 3.4 of reducing, by one third, premature deaths from NCDs by 2030, and outlines the disparities in progress on preventing NCDs worldwide.
This toolkit is a “how to” guide for developing, implementing and evaluating a multisectoral action plan for prevention and control of NCDs. It is targeted at policy-makers, planners and programme managers, and is intended to help countries, provinces and cities meet the requirements for achieving global and national NCD targets and the Sustainable Development Goals.
The toolkit takes the user through a series of actions related to the development of a multisectoral action plan (“MSAP development actions”), and provides forms and a template framework for users to complete as they undertake these actions.
Developing a multisectoral action plan involves establishing health needs and engaging relevant stakeholders before determining the actions to take, identifying and prioritizing interventions, deciding on ways to address NCDs while establishing support and resources for prevention and control, and evaluating progress in implementing the plan.
Using the toolkit is an inclusive and participatory process that involves engaging relevant stakeholders before determining the actions to take. The toolkit focuses on the main NCDs and wider determinants of health and aims to reduce the premature mortality from NCDs and the negative impacts of these determinants on health and health inequalities.
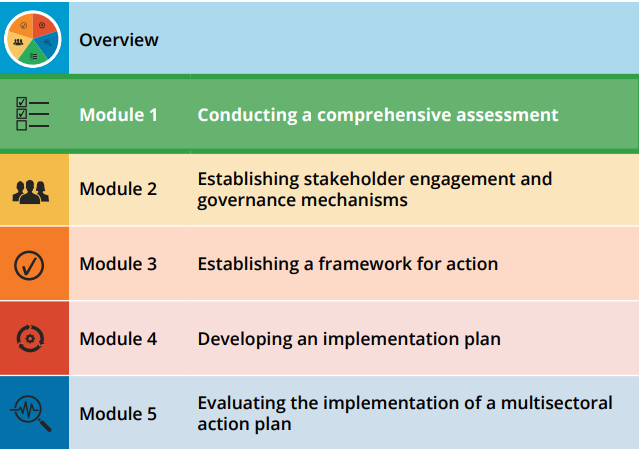
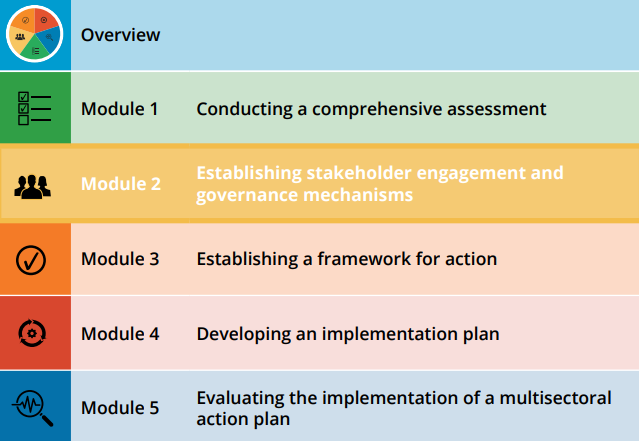
This work entails an array of competencies, such as situation analysis, advocacy, planning, mobilizing, implementing interventions and evaluating them, and disseminating the results of the evaluation. Users can refer to programme theory and logic modelling to guide the development of their action plan. The structure of the toolkit is set out in Fig. 1.1.
Fig. 1.1 Structure of the toolkit for developing a multisectoral action plan for noncommunicable diseases
One of the first steps in developing a multisectoral action plan (MSAP) is to use a situation analysis to provide a comprehensive assessment of the health needs, prevailing risks and the context of the area to which the plan will apply. This will help countries, regions, provinces or cities intending to create a multisectoral action plan to align with the global commitments on targeting the four major NCDs: cardiovascular disease, diabetes, cancer and chronic respiratory diseases.
A situation analysis is essentially an information-gathering process to understand the specifics of the NCD burden in a particular area, as well as the nature and extent of any activities that may be in place to deal with the problem. It is therefore a critical component of the development of any policy, plans and programmes designed to address NCD prevention and control.
A situation analysis guides the identification of priorities for an action plan and informs the subsequent steps in the planning process. It should therefore be conducted before developing an NCD strategy or plan. It seeks to establish a clear, detailed and realistic picture of the opportunities, resources, challenges and barriers regarding NCDs and their determinants.
A systematic situation analysis is an essential component of building the case; it is only through such an analysis that the needs, gaps and country capacity for, and response to, NCD prevention and control can be documented and understood. In addition, the results of the analysis provide the essential baseline data necessary for planning, monitoring and evaluating any policy or programme interventions.
The quality of the situation analysis will affect the success of the entire national effort for NCD prevention and control.
The epidemic of NCDs is being driven by powerful forces, including demographic ageing, rapid unplanned urbanization, and the globalization of unhealthy lifestyles. NCDs and their risk factors are unevenly distributed within populations, and these inequalities need to be considered to ensure an effective mix of policy solutions is selected.
Population and health indicators
Health indicators are quantifiable characteristics of a population. These include, but are not limited to, population growth, crude birth rates, age-adjusted death rates, maternal mortality ratios, female/male populations and infant mortality rates. Such basic information should be included when assessing the health status of a population.
Economic and health indicators
Economic and health expenditure indicators include, but are not limited to, gross national income (GNI), inflation rate and health expenditure.
Social determinants of health
The social determinants of health are the circumstances in which people are born, grow, live, work and age, and the systems put in place to deal with illness. These circumstances are, in turn, shaped by a wide set of forces that includes economics, social policies and politics. Better health contributes to increased well-being, education, social cohesion, environmental protection, increased productivity and economic development. A “virtuous circle” is thus possible whereby improvements in health and its determinants feed back into each other, providing mutual benefits.
NCDs cannot be addressed effectively without action on social determinants of health. For example, local transport and housing policies are needed, as are national fiscal, environmental, education and social policies, along with global financial, trade and agriculture policies. Understanding and modifying the social determinants of NCDs is crucial to addressing inequalities in NCDs and in health outcomes between different social groups.
Social determinants need to be routinely monitored and factored into policy-making in order to evaluate the impact of policies and change course when necessary.
Table 1:Example of population and health indicators
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–20
NCDs have been established as a clear threat, not only to human health, but also to development and economic growth. NCDs are the leading cause of death globally, responsible for more than 70% of all deaths. Almost three quarters of NCD deaths occur in low- and middle-income countries and, of these deaths, 85% are “premature”: of people aged between 30 and 69 years (4). The disability caused by chronic illness, and the lives lost, are endangering industrial competitiveness across borders
The global response to NCDs has included the UN High-level meetings of 2011 and 2018 and the declarations resulting from them (1, 5). In addition, Sustainable Development Goal target 3.4 commits to reducing, by one third, premature deaths from NCDs by 2030.
To determine the magnitude of the NCD problem in each country, region, province or city, the following information is required:
— mortality rates attributable to each of the four leading NCDs: cardiovascular disease, diabetes, cancer, and chronic respiratory diseases;
— age-standardized rates and gender-specific data concerning mortality and morbidity;
— overall premature NCD mortality rates;
— prevalence of multiple risk factors in the population, such as unhealthy diets, harmful use of tobacco and lack of physical activity;
— further breakdown by ethnicity, income, education, geographical location (regional or local) to identify highly affected and vulnerable groups (if available);
— trends (if available); and
— overall impact of NCDs on development and social burdens.
Mortality
Mortality data indicate the number of deaths by place, time and cause. The methodology used to measure mortality depends on the capacity of the country. Strengthening vital registration is essential to achieving quality mortality data. However, where vital registration is unavailable, or inadequate, from the perspective of coverage and/or quality, it is acceptable to use alternative methods, such as verbal autopsy.
Morbidity
Morbidity data provide important information for the management of health care systems, in particular the planning and evaluation of service delivery. They are useful for the estimation of disease burden, gaps in health system capacity, and the identification of missed opportunities in prevention. They also provide critical information for the evaluation of quality of care, and the production of cost estimates of NCDs to the health system and individuals.
The principal methods for collecting morbidity data include population- based disease registries, hospital-based registries, cross-sectional surveys, cohort studies and technology that links records routinely collected by health and administrative data systems.
Cancer registries are important because cancer type and staging are critical in the planning of health care services, and to the quality of care assessment and prevention programmes. For this reason, cancer registration has been included in the global NCD monitoring framework. The inclusion of indicators of acute myocardial infarction, stroke, chronic obstructive pulmonary disease (COPD), asthma, diabetes, and kidney and liver disease will depend on a country’s technical and economic capacity, as well as the priority assigned to these conditions. Surveys and/or hospital- based data are recommended for these morbidity indicators.
Data sources
Disease incidence can be assessed through population-based disease registries and/or hospital-based registries, where feasible. Record linkage can be used to calculate incidence from routinely collected health and administrative data systems. Prevalence rates of the main NCD risk factors can be assessed through WHO STEPS surveys, tobacco surveys or similar health surveys representative of the national or sub-national levels. Case fatality and survival rates are derived from statistical analysis of disease registry and hospital-based data. (See Resources section.)
Risk and protective factors
NCDs are complex and multifactorial. The main risk factors linked to the four most prevalent NCDs are:
— tobacco use
— unhealthy diet
— physical inactivity
— the harmful use of alcohol.
These risk factors have their roots in unhealthy patterns of living, and the environments where people live, play and work. It is recommended that the plan takes into account the prevalence of these risk factors.
Table 2 Example of economic and health expenditure indicators
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
A critical component of a situation analysis is to gather as much relevant information as possible to establish a level of understanding of current activities being undertaken with respect to NCD prevention and control. Assessing the nature and extent of activities (or the lack thereof) across sectors is important for a national or regional situation analysis. The sections below describe the key elements to consider.
2.3.1 Interventions, experience and best practices
A desk review could be conducted to examine the best practices and experience in prevention and control of NCDs, consistent with the technical and financial capacity available. This review should seek to:
— assess the existing evidence-based interventions and experience in the prevention and control of NCDs, including community-based programmes;
— identify procedures and practices used to deliver health services;
— review the influence of NCDs on economic and social development;
— identify major issues and key gaps in knowledge, resources and management that need to be addressed to move forward the national NCD prevention and control agenda;
— provide information and guidance on developing, implementing and evaluating sustainable and effective national NCD prevention and control policies and programmes; and
— integrate NCDs and risk factors into master health plans and synchronize them with well-established programmes such as those addressing HIV/AIDS and tuberculosis (TB).
2.3.2 National NCD strategies, policies, programmes and plans
An important component of a situation analysis is an examination of the status of existing NCD-relevant policies, strategies, action plans, programmes and guidelines. This could include:
— legislation, regulations and ministerial decrees;
— overarching national health and development strategies;
— use of pre-existing and well-established plans on communicable diseases, such as HIV/AIDS and TB;
— polices, strategies, plans, programmes and guidelines formulated and implemented by the ministry of health (MoH) in response to NCD prevention and control;
— use of a multisectoral action plan for NCDs in existing master or developmental plans, along with sustained national commitments;
— policies, strategies, plans and programmes originating in other government ministries, such as those involved in transportation, agriculture, education and finance that have significant impact (both negative and positive) on population health and NCDs; and
— technical guidelines.
2.3.3 Capacity of the health system for NCD prevention and control
Health service
An assessment of health sector capacity is key to determining its ability to tackle NCD prevention and control. It is important to consider the capacities of both the public and the private health sector in relation to NCD prevention and management. For both, the following components require assessment:
— physical and organizational infrastructure
— appropriate equipment, medicines and technology
— numbers and extent of training of appropriate personnel
— availability of practice guidelines for specific NCD conditions and risk factor management
— distribution of services and personnel
— access to services with regard to chronic conditions.
Assessment of primary care services is also required, in terms of:
— health promotion and primary prevention
— surveillance
— management of risk factors
— treatment of the main NCDs
— palliative care and home-based care
— patient education, self-care
— counselling.
Health information systems
A situation analysis is necessary to assess the extent to which health information systems can deliver quality data, applicable to the jurisdiction involved. An assessment of the capacity to use and analyse existing data is also an important element.
National health information comes principally from the following resources: a national health reporting system, a disease registry system, regular or irregular surveys, and surveillance on mortality or morbidity of specific diseases or prevalence of risk factors.
Financial resources
A situation analysis should consider the potential sources of financial resources to support NCD policies and programmes and the potential for financial and in-kind support from other sectors and stakeholders that have an interest in health, such as:
— government departments and agencies
— international and national NGOs
— national and international philanthropic organizations
— research funding agencies
— health charities
— private sector, e.g. insurance companies.
Research capacity
A national NCD policy and a plan need to be informed by evidence. Addressing gaps in this evidence can be greatly assisted by applied, policydriven research. A situation analysis should therefore include, as far as possible, an assessment of research capacity that could potentially be harnessed to support NCD prevention and control.
A situation analysis can include an assessment of basic clinical, epidemiological and implementation research, and can target particular population groups and settings. The analysis should also provide information on possible gaps in research training, methodology development and how research results are used and disseminated. In particular, research capacity includes research on methods and theories of implementation that can be applied to identify gaps in implementation of the existing evidence-based interventions, technical guidelines and barriers, and facilitators. Research can also help to develop implementation strategies to address these issues in order to improve the implementation.
Community capacity
Assessment of community capacity includes the following areas:
— public awareness and health literacy with regard to NCD prevention and control;
— the existence of supportive networks, for example patient associations;
— the existence of supportive local environments, for example school programmes and municipal or local initiatives and facilities, including recreational facilities;
— a supply of supportive services, including water supply and sanitation;
— adequate safety measures in the local environment; and
— the existence of community leaders and champions to help motivate behavioural change.
2.3.4 Responses of non-health sectors
NCD prevention and control requires a range of actors for an effective response. At the national level, multi-stakeholder collaborations and partnerships are vital because in most national and local budgets resources for the prevention and control of NCDs are limited. An assessment of contributions by non-health sectors to NCD prevention and control include the following areas:
— the existence of partnerships or collaborations for implementing key NCD activities at the national level, such as advocacy and awareness- raising, financing and resource mobilization, capacity-building, and product development and innovation;
— existing mechanisms for cooperation and coordination among relevant sectors;
— descriptions of NGOs, private sectors, charitable organizations, foundations, etc., in terms of their networks, involvement, activities, contributions, interests and impacts.
Table 2 Example of economic and health expenditure indicators
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
This situation analysis is paramount to the success of developing a plan as it underpins the stakeholders’ assessment of the opportunities, resources, challenges and barriers regarding NCDs, and the relevance and importance of the available interventions. Furthermore, the situation analysis serves as a baseline when monitoring and evaluating the interventions implemented as a result of the plan.
Before embarking on the process of developing a multisectoral action plan, the responsible officer therefore needs to gather the necessary information and provide a summary of the situation – including the NCD burden, capacity, major socioeconomic policies and the addressing of health issues in a range of policies. This profile of the country/province/ city should also identify weaknesses, strengths and challenges faced when reinforcing NCD prevention and control.
A more detailed analysis may be required for a specific programme, including epidemiological data and national capacity in the area of the specific programme, and social acceptability for the planned intervention. For example, in a national tobacco control programme, it is important to know the prevalence of current smokers in different population groups. This includes types of tobacco used; advertising and promotion restrictions; prices of various types of tobacco; existing legislations to control tobacco, including exposure to second-hand smoke and cessation practices; the burden of diseases related to tobacco; and national progress towards the implementation of the WHO Framework Convention on Tobacco Control (FCTC).
Table 2 Example of economic and health expenditure indicators
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
MSAP DEVELOPMENT ACTION 1: Prepare a situation analysis and summary
Key Messages
— Teams developing a multisectoral action plan for NCDs should include the four main NCDs in their plan: CVD, diabetes, cancer, and chronic respiratory disease.
— A situation analysis of the NCD burden and activities that may be in place to deal with the problem is a critical component of developing a country action plan.
— Age- and sex-specific data concerning mortality and morbidity are the mainstay of information systems to determine the size of the NCD burden. Wherever possible, data should be analysed by socio-economic status, ethnicity and other relevant variables to assess inequalities in NCDs.
— The population prevalence of NCD risk factors, including unhealthy diets, use of tobacco, harmful use of alcohol and lack of physical activity, must be considered.
— A critical component of a situation analysis is to gather information on current activities, master health plans, development plans, and individual health plans being undertaken, and to integrate NCDs and their risk factors into those ongoing responses.
— In order to harness the collective capacity of all stakeholders who have an influence on a community’s determinants of health, it is important to identify them.
— A situation analysis provides essential baseline data necessary for the planning, monitoring and evaluation of any policy and programme intervention.
— A situation analysis needs a summary of all information gathered.
NCDs have been established as a clear threat, not only to human health, but also to development and economic growth. NCDs are the leading cause of death globally, responsible for more than 70% of all deaths. Almost three quarters of NCD deaths occur in low- and middle-income countries and, of these deaths, 85% are “premature”: of people aged between 30 and 69 years (2). The disability caused by chronic illness, and the lives lost, are endangering industrial competitiveness across borders. The global response to NCDs has included the UN High-level meetings of 2011 and 2018 and the declarations resulting from them (3, 4). In addition, Sustainable Development Goal target 3.4 commits to reducing, by one third, premature deaths from NCDs by 2030.
To determine the magnitude of the NCD problem in each country, region, province or city, the following information is required:
— mortality rates attributable to each of the four leading NCDs: cardiovascular disease, diabetes, cancer, and chronic respiratory diseases
— age-standardized rates and gender-specific data concerning mortality and morbidity
— overall premature NCD mortality rates
— prevalence of multiple risk factors in the population, such as unhealthy diets, harmful use of tobacco and lack of physical activity
— further breakdown by ethnicity, income, education, geographical location (regional or local) to identify highly affected and vulnerable groups (if available)
— trends (if available); and
— overall impact of NCDs on development and social burdens.
Mortality data indicate the number of deaths by place, time and cause. The methodology used to measure mortality depends on the capacity of the country. Strengthening vital registration is essential to achieving quality mortality data. However, where vital registration is unavailable, or inadequate, from the perspective of coverage and/or quality, it is acceptable to use alternative methods, such as verbal autopsy.
Table 3 :Example of leading causes of death (or morbidity where mortality data are not available)*
The United Nations Population Division (2009). World population prospects: the 2008 revision
WHO (2008) The global burden of disease: 2004 update
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
Morbidity data provide important information for the management of health care systems, in particular the planning and evaluation of service delivery. They are useful for the estimation of disease burden, gaps in health system capacity, and the identification of missed opportunities in prevention. They also provide critical information for the evaluation of quality of care, and the production of cost estimates of NCDs to the health system and individuals.
The principal methods for collecting morbidity data include population-based disease registries, hospital-based registries, cross-sectional surveys, cohort studies and technology that links records routinely collected by health and administrative data systems.
Cancer registries are important because cancer type and staging are critical in the planning of health care services, and to the quality of care assessment and prevention programmes. For this reason, cancer registration has been included in the global NCD monitoring framework. The inclusion of indicators of acute myocardial infarction, stroke, chronic obstructive pulmonary disease (COPD), asthma, diabetes, and kidney and liver disease will depend on a country’s technical and economic capacity, as well as the priority assigned to these conditions. Surveys and/or hospital-based data are recommended for these morbidity indicators
WHO global monitoring framework
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
Data sources
Disease incidence can be assessed through population-based disease registries and/or hospital-based registries, where feasible. Record linkage can be used to calculate incidence from routinely collected health and administrative data systems. Prevalence rates of the main NCD risk factors can be assessed through WHO STEPS surveys, tobacco surveys or similar health surveys representative of the national or sub-national levels. Case fatality and survival rates are derived from statistical analysis of disease registry and hospital-based data. (See Resources section.)
WHO global monitoring framework
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
NCDs are complex and multifactorial. The main risk factors linked to the four most prevalent NCDs are: — tobacco use — unhealthy diet — physical inactivity — the harmful use of alcohol. These risk factors have their roots in unhealthy patterns of living, and the environments where people live, play and work. It is recommended that the MSAP takes into account the prevalence of these risk factors.
WHO global monitoring framework
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
A critical component of a situation analysis is to gather as much relevant information as possible to establish a level of understanding of current activities being undertaken with respect to NCD prevention and control. Assessing the nature and extent of activities (or the lack thereof) across sectors is important for a national or regional situation analysis. The sections below describe the key elements to consider. 1.3.1 Interventions, experience and best practices A desk review could be conducted to examine the best practices and experience in prevention and control of NCDs, consistent with the technical and financial capacity available. This review should seek to: — assess the existing evidence-based interventions and experience in the prevention and control of NCDs, including community-based programmes; — identify procedures and practices used to deliver health services; — review the influence of NCDs on economic and social development; — identify major issues and key gaps in knowledge, resources and management that need to be addressed to move forward the national NCD prevention and control agenda; — provide information and guidance on developing, implementing and evaluating sustainable and effective national NCD prevention and control policies and programmes; and — integrate NCDs and risk factors into master health plans and synchronise them with well-established programmes such as those addressing HIV/AIDS and tuberculosis (TB).
Table 4:Example of prevalence (%) of risk factors
WHO Global Health Observatory (GHO) data
WHO global monitoring framework
WHO Expert Committee on Problems Related to Alcohol Consumption
WHO Global database on the implementation of nutrition action (GINA)
Global status report on alcohol and health 2014
WHO (2013). Global nutrition policy review: what does it take to scale up nutrition action?
WHO (2009). Interventions on diet and physical activity: what works. Summary report
A critical component of a situation analysis is to gather as much relevant information as possible to establish a level of understanding of current activities being undertaken with respect to NCD prevention and control. Assessing the nature and extent of activities (or the lack thereof) across sectors is important for a national or regional situation analysis. The sections below describe the key elements to consider.
Desk review
A desk review could be conducted to examine the best practices and experience in prevention and control of NCDs, consistent with the technical and financial capacity available. This review should seek to:
- assess the existing evidence-based interventions and experience in the prevention and control of NCDs, including community-based programmes;
- identify procedures and practices used to deliver health services
- review the influence of NCDs on economic and social development
- identify major issues and key gaps in knowledge, resources and management that need to be addressed to move forward the national NCD prevention and control agenda
- provide information and guidance on developing, implementing and evaluating sustainable and effective national NCD prevention and control policies and programmes; and
- integrate NCDs and risk factors into master health plans and synchronise them with well-established programmes such as those addressing HIV/AIDS and tuberculosis (TB).
Key Messages
— Teams developing an MSAP for NCDs should include the four main NCDs in their plan: CVD, diabetes, cancer, and chronic respiratory disease.
— A situation analysis of the NCD burden and activities that may be in place to deal with the problem is a critical component of developing a country action plan.
— Age- and sex-specific data concerning mortality and morbidity are the mainstay of information systems to determine the size of the NCD burden. Wherever possible, data should be analysed by socio-economic status, ethnicity and other relevant variables to assess inequalities in NCDs.
— The population prevalence of NCD risk factors, including unhealthy diets, use of tobacco, harmful use of alcohol and lack of physical activity, must be considered.
— A critical component of a situation analysis is to gather information on current activities, master health plans, development plans, and individual health plans being undertaken, and to integrate NCDs and their risk factors into those ongoing responses.
— In order to harness the collective capacity of all stakeholders who have an influence on a community’s determinants of health, it is important to identify them.
— A situation analysis provides essential baseline data necessary for the planning, monitoring and evaluation of any policy and programme intervention.
— A situation analysis needs a summary of all information gathered.
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
WHO Cost effectiveness and strategic planning (WHO-CHOICE)
Health in All Policies--Seizing opportunities, implementing policies
An important component of a situation analysis is an examination of the status of existing NCD-relevant policies, strategies, action plans, programmes and guidelines. This could include:
- legislation, regulations and ministerial decrees;
- overarching national health and development strategies;
- use of preexisting and well-established plans on communicable diseases, such as HIV and TB plans
- polices, strategies, plans, programmes and guidelines formulated and implemented by the Ministry of Health (MOH) in response to NCD prevention and control;
- use of NCD MSAP in existing master plans, developmental plans, and sustained national commitments
- policies, strategies, plans and programmes originating in other government ministries, such as those involved in transportation, agriculture, education and finance that have significant impact (both negative and positive) on population health and NCDs;
- technical guidelines.
Assessing national capacity for the prevention and control of NCDs
WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–20
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
Health in All Policies--Seizing opportunities, implementing policies
Health service
An assessment of health sector capacity is key to determining a country’s ability to tackle NCD prevention and control. It is important to consider the capacities of both the public and the private health sector in relation to NCD prevention and management. For both, the following components require assessment:
- physical and organizational infrastructure
- appropriate equipment, medicines and technology
- numbers and extent of training of appropriate personnel
- availability of practice guidelines for specific NCD conditions and risk factor management
- distribution of services and personnel
- access to services with regard to chronic conditions.
Assessment of primary care services is also required, in terms of:
- health promotion and primary prevention
- surveillance
- management of risk factors
- treatment of the main NCDs
- palliative care and home-based care;
- patient education, self-care
- counselling.
Health information systems
A situation analysis needs to assess the extent to which health information systems can deliver quality data, applicable to the jurisdiction involved. In addition, an assessment of the capacity to use and analyse existing data is an important element.
National health information comes principally from the following resources: a national health reporting system; a disease registry system; regular or irregular surveys; and surveillance on mortality or morbidity of specific diseases or prevalence of risk factors.
Financial resources
A situation analysis should consider the potential sources of financial resources to support NCD policies and programmes and the potential for financial and in-kind support from other sectors and stakeholders that have an interest in health, such as:
- government departments and agencies
- international and national NGOs
- national and international philanthropic organizations
- research funding agencies
- health charities
- private sector, e.g. insurance companies.
Research capacity
A national NCD policy and plan need to be evidence-informed. Addressing gaps in this evidence can be greatly assisted by applied policy-driven research. Therefore, to the extent feasible, a situation analysis should include an assessment of research capacity that could potentially be harnessed to support NCD prevention and control.
Research and research requirements are country specific. Integral are the relationship and links between the research community, decision-makers and administrators, i.e. those who require evidence to inform the gaps identified, for example in a situation analysis. A situation analysis can include the assessment of basic, clinical, epidemiological and operational research, and can target particular population groups and settings. The analysis should also provide information on possible gaps in research training, methodology development and how research results are used and disseminated.
Community capacity
Assessment of community capacity includes the following areas:
- public awareness and health literacy with regard to NCD prevention and control;
- the existence of supportive networks, for example patient associations;
- the existence of supportive local environments, for example school programmes and municipal or local initiatives and facilities, including recreational facilities;
- a supply of supportive services, including water supply and sanitation;
- adequate safety measures in the local environment;
- the existence of community leaders and champions to help motivate behavioural change.
Table 5:Example of human resources available for NCD prevention and control
Table 6:Example of financial allocation for health and NCD prevention and control
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
NCD prevention and control require a range of actors for an effective response. At the national level, multi-stakeholder collaborations and partnerships are vital because, in most national and local budgets, resources for the prevention and control of NCDs are limited. An assessment of contributions by non-health sectors to NCD prevention and control include the following areas:
- the existence of partnerships or collaborations for implementing key NCD activities at the national level, such as advocacy and awareness-raising, financing and resource mobilization, capacity-building, and product development and innovation;
- existing mechanisms for cooperation and coordination among relevant sectors;
- descriptions of NGOs, private sectors, charitable organizations, foundations, etc., in terms of their networks, involvement, activities, contributions, interests and impacts
WHO (2011). Global status report on noncommunicable diseases 2010
WHO (2014). Global status report on noncommunicable diseases 2014
This situation analysis is paramount to the success of developing an MSAP as it underpins the stakeholders’ assessment of the opportunities, resources, challenges and barriers regarding NCDs, and the relevance and importance of the available interventions. Furthermore, the situation analysis serves as a baseline when monitoring and evaluating the interventions implemented as a result of the MSAP.
Before embarking on the process of developing an MSAP in modules 3, 4 and 5, the responsible officer therefore needs to gather the necessary information and provide a summary of the situation – including the NCD burden, capacity, major socioeconomic policies and the addressing of health issues in a range of policies. This profile of the country/province/ city should also identify weaknesses, strengths and challenges faced when reinforcing NCD prevention and control.
A more detailed analysis may be required for a specific programme, including epidemiological data and national capacity in the area of the specific programme, and social acceptability for the planned intervention. For example, in a national tobacco control programme, it is important to know the prevalence of current smokers in different population groups. This includes types of tobacco used; advertising and promotion restrictions; prices of various types of tobacco; existing legislations to control tobacco, including exposure to second-hand smoke and cessation practices; the burden of diseases related to tobacco; and national progress towards the implementation of the WHO Framework Convention on Tobacco Control (FCTC).
Click here to back to main text
ACTION 1: Prepare a situation analysis and summary
✤ Step 1: Gather the information you need for a situation analysis
— Form 1.1 provides a structure for recording the information.
✤ Step 2: Describe the status of NCDs within your remit and outline a suitable response
— Identify challenges and opportunities to tackle the NCD epidemic.
— Write up your report. A suggested structure is outlined below.
Suggested structure for a situation analysis and summary
Profile of area
— Describe the status of the population and provide the main health indicators.
— Describe the status of economic and health expenditure.
Status and trends of NCDs and their determinants
— Provide information on the status and trends of NCDs, including mortality and morbidity, and the prevalence of their risk factors.
— List the main NCDs and common risk factors.
— Provide the premature death rate (30 to 70 years old) from NCDs.
— List the social determinants for NCDs.
Current responses and commitments
— Put your MSAP in context by including reference to:- global NCD strategies, targets, action plans, and monitoring frameworks;
- regional NCD action plan/framework;
- national efforts to tackle NCDs including NCD strategies, action plans, and programmes;
- health system readiness: the availability of health infrastructures related to NCDs, including public health institutes, health service delivery for NCDs, health information, financial resources and human health resources; and
- the response of the non-health-sector, private sector and NGOs to the NCD epidemic.
Summary of findings and proposals for action
— Identify the most important risk factors.
— Describe barriers and challenges to tackling NCDs and their determinants.
— Identify key gaps in existing policies, actions and research for NCD prevention and control.
— Propose ways in which the MSAP could reduce premature mortality and result in a healthier population.
CHECKLIST
Use the Checklist available here to make sure you have completed all the necessary steps before moving on to the next module.
- Blas E, Sivasankara Kurup A, World Health Organization (WHO), editors (2010). Equity, social determinants and public health programmes. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/44289) .
- Commission on Social Determinants of Health (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Final report: executive summary. Geneva: World Health Organization WHO/IER/CSDH/08.1; (https://apps.who.int/iris/handle/10665/69832) .
- UN (2011). Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations (A/ RES/66/2; ( https://digitallibrary.un.org/record/710899/?ln=en) .
- UN (2018). Political declaration of the Third High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. New York: United Nations (A/RES/73/2; ( https://digitallibrary.un.org/record/1648984?ln=en).
- WHO. Global Health Observatory (GHO) [online database]. Geneva: World Health Organization (https://www.who.int/data/gho/data/themes/noncommunicable-diseases) .
- WHO. Health accounts [online resource]. Geneva: World Health Organization ( https://www.who.int/health-topics/health-accounts#tab=tab_1) .
- WHO. Social determinants of health [website]. Geneva: World Health Organization (https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1,accessed 1 November 2021).
- WHO. STEPwise approach to NCD risk factor surveillance (STEPS) [online tool] (https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps) .
- WHO (2008). 2008–2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. Geneva: World Health Organization (https://www.who.int/nmh/publications/ncd_action_plan_en.pdf) .
- WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–20. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/94384).
- WHO (2018). Time to deliver: report of the WHO Independent High-level Commission on Noncommunicable Diseases. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/272710).
- WHO (2019). Global health estimates [online database]. Geneva: World Health Organization (https://www.who.int/data/global-health-estimates) .
- Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations; 2011 (A/RES/66/2; https://digitallibrary.un.org/record/720106,accessed 1 November 2021).
- Global action plan for the prevention and control of NCDs 2013–2020. Geneva: World Health Organization; 2013 (https://apps.who.int/iris/handle/10665/94384,accessed 1 November 2021) .
- Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014 (http://apps.who.int/iris/handle/10665/148114,accessed 1 November 2021) .
- Noncommunicable diseases: key facts [website]. World Health Organization (https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases,accessed 1 November 2021).
- Political declaration of the third high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations; 2018 (A/RES/73/2; (https://digitallibrary.un.org/record/1648984,accessed 1 November 2021) .
-
Citation
World Health Organization(2022). Toolkit for developing a multisectoral action plan for noncommunicable diseases: module 1: conducting a comprehensive assessment. World Health Organization. https://apps.who.int/iris/handle/10665/353164. License: CC BY-NC-SA 3.0 IGO.
ISBN Module of 1 is -9789240043497 (electronic version)
9789240043503 (print version)
Noncommunicable diseases (NCDs) are the leading cause of death globally, killing more people each year than all other causes combined. Contrary to common perceptions, available data show that nearly 80% of NCD-related deaths occur in low- and middle-income countries. Moreover, recent decades have witnessed a steady increase in such deaths, with vulnerable population groups often worst affected, and yet many of the dire human and social consequences could be prevented by implementing cost-effective and feasible interventions.
The Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases (2011) (1) recognizes the scale of the NCD crisis and the urgent need for action. The Global action plan for the prevention and control of NCDs 2013–2020 (2) , recently extended to 2030, provides a vision and a road map to scale up action for the prevention and control of NCDs.
The global epidemic of NCDs is widely acknowledged as a major challenge to development in the 21st century and is a significant threat to achieving the United Nations Sustainable Development Goals. In addition, globally, the main NCDs represent the greatest cause of death in people aged under 70 years, imposing years of disability on those affected and their families. The Global status report on noncommunicable diseases 2014 (3) highlights the need to intensify national multisectoral action to meet the global targets that governments have agreed upon and to protect people from cardiovascular diseases, cancers, diabetes and chronic respiratory diseases.
Countries, including some that are low-income, are showing that it is feasible to make progress and reduce premature deaths from NCDs. But that progress, particularly in low- and middle-income countries, is insufficient and uneven. The global status report of 2014 reveals a distressing gap in our ability to achieve Sustainable Development Goal target 3.4 of reducing, by one third, premature deaths from NCDs by 2030, and outlines the disparities in progress on preventing NCDs worldwide.
This toolkit is a “how to” guide for developing, implementing and evaluating a multisectoral action plan for prevention and control of NCDs. It is targeted at policy-makers, planners and programme managers, and is intended to help countries, provinces and cities meet the requirements for achieving global and national NCD targets and the Sustainable Development Goals.
The toolkit takes the user through a series of actions related to the development of a multisectoral action plan (“MSAP development actions”), and provides forms and a template framework for users to complete as they undertake these actions.
Developing a multisectoral action plan involves establishing health needs and engaging relevant stakeholders before determining the actions to take, identifying and prioritizing interventions, deciding on ways to address NCDs while establishing support and resources for prevention and control, and evaluating progress in implementing the plan.
Using the toolkit is an inclusive and participatory process that involves engaging relevant stakeholders before determining the actions to take. The toolkit focuses on the main NCDs and wider determinants of health and aims to reduce the premature mortality from NCDs and the negative impacts of these determinants on health and health inequalities.
This work entails an array of competencies, such as situation analysis, advocacy, planning, mobilizing, implementing interventions and evaluating them, and disseminating the results of the evaluation. Users can refer to programme theory and logic modelling to guide the development of their action plan. The structure of the toolkit is set out in Fig. 2.1.
Fig. 2.1 Structure of the toolkit for developing a multisectoral action plan for noncommunicable diseases
This section considers two complementary aspects:
— Stakeholder engagement: identifying the stakeholders to be involved in the development of national NCD policies and programmes and choosing the best methods for engagement.
— Options for multisectoral governance mechanisms: examples of the types of mechanism and structure that can be used to ensure clear leadership, ongoing stakeholder engagement and effective implementation of a national multisectoral NCD strategy or action plan.
To maintain a structured and well-organized implementation plan it is important to have a lead agency or sector. The ministry of health or a similar authority in government will be critical in facilitating development and implementation of the multisectoral action plan. The ministry of health can facilitate multisectoral action through:
— coordinating multiple agencies;
— engaging relevant sectors and optimizing meaningful participation;
— organizing committee meetings;
— following up on decisions made by the coordinating bodies;
— identifying implementation gaps and proposing measures to implement new strategies; and
— preparing consolidated reports.
The roles and responsibilities of the ministry of health and relevant sectors in implementing the plan should be identified and discussed in collaboration with relevant sectors.
A national response to NCDs cannot come from the health sector alone. The Political declaration of the United Nations High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases of 2011 (1) calls for the strengthening and facilitating of multisectoral action for the prevention and control of NCDs through effective partnership. It is critical for Member States to establish a high-level national multisectoral mechanism for planning, guiding, monitoring and evaluating the enactment of a national NCD policy. Due to the complex nature of NCDs and their risk factors, agreement on concepts and solutions from such a diverse range of stakeholders is rarely straightforward. Ensuring that actions included in a multisectoral action plan are clearly linked to a responsible agency or department is also important. The implementation of the strategy needs to be overseen by a body capable of holding the agencies responsible to account.
This section provides the tools and further resources necessary for working out whom to engage with and how to do it. Exactly which stakeholders are engaged, how many there are, and the most successful methods of engagement will depend on the type of policy or programme.
Who is a stakeholder?
A stakeholder is a person, group or organization with some interest or influence in the strategy or action plan. Primary stakeholders or beneficiaries are those who are ultimately affected, such as the community. Secondary stakeholders are people or organizations involved in the implementation of the plan, such as public health practitioners, officials of the ministries of health or education, or employees of nongovernmental organizations.
Why is stakeholder engagement important?
Stakeholder engagement is as an organization’s effort to understand and involve stakeholders and their concerns in its activities and decision- making processes. This is important because it has real benefits for the level of sustainable outcomes, ownership, participation and the achievement of the plan’s goals. Plans and programmes that do not engage with stakeholders run the real risk of not achieving their goals.
A fundamental question when considering stakeholder engagement is: why should stakeholders wish to become involved in the prevention and control of NCDs and the promotion of health and well-being? Stakeholder involvement can result from a mixture of altruism, investment, compulsion or the desire to maintain market position with competitors, or to gain from the potential benefits offered by involvement. Once engaged, it is important to maintain a high level of stakeholder participation and motivation.
The involvement of a broad range of stakeholders in the planning process is critical to promoting multisectoral action for NCD prevention and control. The level to which stakeholders are engaged and the type and methods of engagement can vary in practice. However, in summary, stakeholder identification aims to :
— identify and define the characteristics of key stakeholders;
— assess the manner in which they might affect or be affected by the programme/project outcome;
— understand the relationships between stakeholders, including an assessment of real or potential conflicts of interest and expectation between stakeholders; and
— assess the capacity of different stakeholders to participate.
Who are the key stakeholders in NCD prevention and control?
Key stakeholders include individuals and organizations within health and other sectors whose work is related to broader health issues but who could become partners in NCD prevention and control. Other potential subgroups and members come from national or regional steering committees that support inter-programme and intersectoral work.
Stakeholder subgroups
Some of the key stakeholders will be representatives from the government sector, the private sector and civil society (see Table 2.1)
Table 2.1 Stakeholder subgroups| Public Sector Stakeholders | Private Sector stakeholders | Civil Society Stakeholders |
|---|---|---|
| Ministers and advisors (executive) | Corporations and businesses | Media |
| Civil servants and departments (bureaucratic) | Business associations | Churches/religious institutions |
| Elected representatives ( legislative) | Professional bodies | Schools and Universities |
| Courts (judicial) | Individual business leader | Social movements and advocacy group |
| Political parties | Financial institutions | Trade unions |
| Local government councils | National nongovernmental organizations | |
| Military | International nongovernmental organizations | |
| Quangos and commissions | ||
| International and development bodies (UN, World Bank) |
Capacities and resources of the stakeholders
The capacities and resources of the stakeholders should be itemized, such as the skills, time available, information, finances and experience.
Roles and responsibilities of the stakeholders
The role of the stakeholders in regard to NCD prevention and control will depend on their interest and level of influence, and how this may impact the programme and other stakeholders.
Table 2.2 provides examples of stakeholders and their possible roles within the framework of NCD prevention and control.
Table 2.2 Examples of stakeholder roles and responsibilities*
| Stakeholders | Possible roles |
|---|---|
| Ministry of Health | Coordinate, advocate and facilitate the contribution of other ministries, government agencies and stakeholders; lead and facilitate development of national NCD policy, plans and programmes. |
| Ministry of Agriculture | Ensure national food and agricultural policies promote and protect public health. |
| Ministry of Education | Develop school health policies and programmes that promote healthy diets, physical activity and smoke-free environments. |
| Ministry of Transport | Develop transport policies that promote walking and non-motorized options. |
| Ministry of Finance | Ensure finance is available to support NCD policy implementation; encourage use of fiscal and taxation policies that promote and protect public health. |
| Ministry of Sports | Develop policy for promoting physical activity. |
| Department of Revenue/Customs | Ensure the collection of taxes levied on tobacco and alcohol to achieve the objectives of public health and public finance; ensure the prevention of Illicit trade of tobacco and alcohol and other substance abuse that impacts NCDs. |
| Ministry of Commerce/Departments of Trade, Investment etc. | Ensure the adoption of multilateral and bilateral trade and investment instruments that are compliant with all global health laws and keep the health of citizens as a priority. |
| Ministry of Consumer Affairs/Information and Broadcasting/Public Affairs | Ensure the dissemination of relevant public health information to all stakeholders through appropriate means, including through packaging and labelling of products and public service announcements. |
| Ministry of Labour/Employment | Ensure the adoption of labour laws that encourage public health measures promoting healthy lifestyles at workplaces; ensure the generation of alternative livelihoods to workers engaged in tobacco growing or in related enterprises that are likely to be impacted by the full implementation of public health policies on NCDs. |
| Ministry of Urban Development | Ensures the development of building codes and town plans that keep a public health focus. |
| Ministry of Foreign Affairs | Negotiate, analyse and ensure adoption of normative international agreements and frameworks that may be directly linked to public health-related issues. |
| Nongovernmental organizations | Advocate action to prevent NCDs, mobilize community support, organize information and education campaigns and deliver NCD services. |
| Civil society | Create expectations for government and the private sector to take action. |
| Academic institutions | Provide expert advice on public health, NCD risk factors and cost-effective interventions. |
| Health professionals | Advocate action, provide clinical and public health information, and support policy and planning processes; assist in implementation of plans and programmes. |
| Media | Provide sustained news coverage of chronic disease prevention to help raise awareness, promote discussion and facilitate change; journalists can be key stakeholders for advocacy and public education in NCD prevention. |
| The private sector when there is no conflict of interest and excluding the tobacco industry. |
Take measures to implement the World Health Organization set of recommendations to reduce the impact of the marketing of unhealthy foods and non-alcoholic beverages to children, while taking into account existing national legislation and policies Consider producing and promoting more food products consistent with a healthy diet, including by reformulating products to provide healthier options that are affordable and accessible and that follow relevant nutrition facts and labelling standards, including information on sugars, salt and fats and, where appropriate, trans fat content. Promote and create an enabling environment for healthy behaviours among workers, including by establishing tobacco-free workplaces and safe and healthy working environments through occupational safety and health measures, including, where appropriate, through good corporate practices, workplace wellness programmes and health insurance plans. Work towards reducing the use of salt in the food industry in order to lower sodium consumption. Contribute to efforts to improve access to and affordability of medicines and technologies in the prevention and control of NCDs. |
*Adapted from Global action plan for the prevention and control of NCDs,Appendix 5 (2).
Networks
Networks are important because each stakeholder may be part of several NCD prevention and control related networks or other non-NCD programmes. Networks also help to strengthen the participant- and resource-base and to build the knowledge, skills and competencies of its members. Networks offer both individuals and organizations the opportunity to better access complementary resources and expertise and their development can be facilitated through agencies.
Timeframe
The timeframe required for stakeholder identification and analysis depends on the speed of information gathering and the selection of the new stakeholders. Adequate time should be allowed for the preparatory stage in order to understand the stakeholder dynamics and to identify the key groups and institutions to be included as a priority.
MSAP DEVELOPMENT ACTION 2: Draw up a list of stakeholders
MSAP DEVELOPMENT ACTION 3: Assess the relative importance of stakeholders
Establishing an engagement strategy
The first step is to develop a strategy for how best to engage with the different stakeholders and to maintain participation and motivation for NCD prevention and control programmes. Key questions to ask are as follows:
— Are the interests of all partners represented?
— Among the stakeholders, are various disciplines represented, e.g. NCDs, risk factors, health service delivery, biomedical sciences, economics, other social sciences, education, public health?
— Are policy-makers adequately represented?
o If so, what level of representation?
o Are you happy with the quality of representation? Top decision-makers are generally too busy to act as representatives and their replacements are often less effective in the role.
o If the quality of representation is not satisfactory, what mechanism is in place to ensure credible representation from the top?
— Are the private sector and NGOs adequately represented?It may be necessary to obtain a listing of all private sectors including private health-care providers and NGOs working in health to ensure adequate representation. However, tobacco, alcohol and food industry and pharma are not be part of policy making in order to avoid conflicts of interests.
— Is there sufficient community representation?It is important to avoid accrediting an elite minority that ignores the needs of the poor, illiterate, women, children and other disadvantaged groups.
Methods for engaging stakeholders
Many methods and tools exist for engaging stakeholders, including public meetings, focus groups, workshops, one-on-one interviews, telephone interviews and questionnaires, and websites.
MSAP DEVELOPMENT ACTION 4: Engage stakeholders
It is critical to establish a high-level multisectoral mechanism at national and local levels for planning, guiding, monitoring and evaluating the enactment of national policy with the effective involvement of sectors outside health. Engagement of stakeholders does not stop with the approval of a national strategy. It is crucial to consider what type of governance mechanisms or structures will be required to ensure that the activities and objectives of the strategy can be put into practice.
This section describes some of the options for governance mechanisms and structures, to ensure clear leadership, ongoing stakeholder engagement and effective implementation of a national multisectoral NCD strategy or action plan.
Under the coordination mechanism, a scientific committee and working group should be considered to provide advice and manage day-to-day implementation of the multisectoral action plan.
A variety of mechanisms and structures can be used for NCD prevention and control activities that involve a range of stakeholders.
— Ministerial linkages - This refers to working together at cabinet level, through a variety of structures and processes. Ministerial linkages can vary in intensity and duration, and encompass activity beyond the regular joint decision-making at cabinet level. They can comprise all, or a select number of, ministers and may focus on a single policy issue or the entire government portfolio. Leadership may reside either with the prime minister or another minister.
— Cabinet committees and secretaries - Some governments may use more informal mechanisms to facilitate cross-departmental engagement. Cabinet committees are recognized for being able to facilitate dialogue and reach agreement on shared policy issues. Cabinet secretariats coordinate and facilitate collective decision-making on behalf of all government ministers.
— Parliamentary committees - Parliaments can contribute to multisectoral action on NCDs through the formation of parliamentary committees. All-party parliamentary committees encourage a more consensual approach. They can enhance the potential influence of findings and support the longevity of an issue as a political priority, despite a change of government.
— Interdepartmental committees and units - These operate at the bureaucratic level and aim to re-orient ministries around a shared priority. Both interdepartmental committees and units usually comprise civil servants. The appeal of such committees and units is that they provide a unique forum for problem solving and debate, which, in turn, lowers implementation costs by involving affected departments in decision-making.
— Joint budgeting - Whether mandatory or voluntary in nature, joint budgeting involves some kind of pooling of government financial resources. This is particularly attractive within the context of engaging action for health in departments which do not have a dedicated budget for cross-cutting health issues. Many joint budgeting initiatives to date have focused on addressing the needs of easily identifiable population groups.
— Delegated financing - This is an example of financing beyond government, usually secured by legislation and distributed to a semi-autonomous statutory body, for example a health promotion agency. Delegated financing can provide funds for intersectoral programmes and projects.
— Public engagement - Public engagement is often used against a backdrop of dissatisfaction at traditional policy-making, particularly in some of the complex public health debates.
— Stakeholder engagement - This is a collaborative governance action initiated by public agencies or institutions and formally includes non-state actors directly in decision-making.
— Public-private partnerships (PPPs) - The establishment of PPPs as governance structures creates relationships between industry and the public sector. This can include the establishment of PPPs which combine industry, government and civil society interests (e.g. the European Union platform for action on diet, physical activity and health). PPPs often develop to meet a particular health challenge and generally seek to improve some aspect of health infrastructure.
Subnational and local coordination mechanisms are also important to support and supervise implementation of a multisectoral action plan.
Countries will need to consider the suitability of these models in their own national context. Multiple options can be pursued simultaneously. More detailed information can be found in the Resources section. In some countries, the mechanisms may need formal support in the form of a law or regulation regarding the composition and functioning of the mechanism, to facilitate the processes of decision-making, collaboration and coordination. A budget will also be required for its work.
Developing a coordination mechanism where there is no existing structure to build on involves the health authority initially convening a cross-sectoral steering group with the capacity to both influence responses from the health sector and other sectors, and for monitoring and evaluation. The steering group can also make recommendations for national or regional structures, as well as for processes to be developed and outcomes to be expected.
After a mechanism has been established, its success depends on its capacity to convince decision-makers of the benefits of pursuing comprehensive and integrated approaches to NCD prevention and control. This can be facilitated by giving support to the steering group in the form of “political will” and “financial flexibility”.
In some countries, the main structures for NCD prevention and control commonly include:
— an NCD unit/department (usually in the MoH);
— technical working groups/taskforces;
— a steering Committee (either chaired by the MOH or higher level of government such as the department of the prime minister); and
— a scientific or expert Committee.
An NCD unit or department can be responsible for advancing the development or revision of NCD prevention and control policies, plans or programmes. These responsibilities include:
— leading, overseeing and coordinating the process;
— providing technical and secretarial support;
— developing background information to inform the planning process e.g. the situation and response to NCD in the country;
— coordinating, networking and mobilizing other ministries and agencies; and
— establishing implementation, dissemination and evaluation mechanisms.
An example of a structure for national NCD control and prevention is set out in Fig.2.2.
Fig.2.2 An example of an NCD prevention and control structure
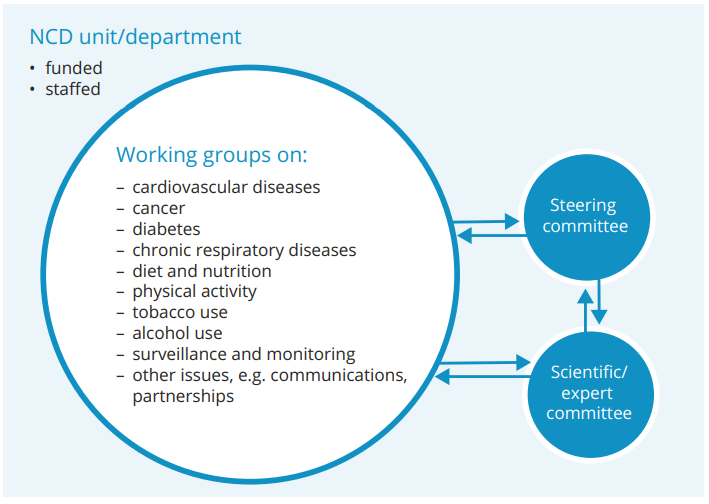
Working groups or taskforces are technical groups which are formulated to perform specific tasks relative to the development and implementation of the policy, plans and programmes. For example, groups may be formed for the development of the National Cancer Control Programme or drafting a National Obesity Control Action Plan.
A Steering Committee, with multisectoral membership, requires terms of reference such as: purpose, objectives, roles and responsibilities, and a declaration of any conflicts of interest among members. The committee may be chaired by a high official of the MoH, or from an office above the ministry level (e.g. the department of the prime minister or deputy prime minister). Functions of the committee include:
— setting national goals and objectives for NCD prevention and control;
— guiding the process of policy, plans and programme development;
— selecting national strategies for NCD prevention and control;
— identifying operational and other resource requirements, and setting priorities;
— guiding and approving the work plans of working groups;
— ensuring the full engagement of partners as well as broad advocacy and communication;
— overseeing the optimal use of existing resources and undertaking resource mobilization for programme implementation and research;
— monitoring progress of the partnership towards established goals (the impact and coverage of cost-effective interventions).
While considering membership of the National Steering Committee, it is important to think about the range of key players who know and care about the NCD problem. Membership could include:
— other government ministries and regulatory agencies, such as agriculture, transportation, education finance, trade and industry, justice, education, employment, environment, housing, and social welfare;
— other professions, for instance legal professions, social workers, community development professionals, health economists, media professionals, administrative staff;
— health care administrators such as hospital and clinic managers of the public and private sector responsible for screening and providing clinical care to those with established chronic disease;
— advocacy groups representing the interests of people with established chronic disease or disadvantaged population groups;
— nongovernmental organizations such as disease and risk factor organizations;and
— operational and front line staff.
Scientific or Expert Committees typically include individuals from service sectors and academic institutions who have expertise in the specific subject under consideration. Membership should be balanced to include experts from medical and social science backgrounds as well as research, with individuals relevant to NCDs and their determinants.For example, members of a scientific/expert committee on a national diabetes prevention and control programme could comprise:
— NCD coordinator (NCD unit)
— clinical experts in diabetes management from major hospitals
— social scientist
— health researcher
— psychologist
— podiatrist from secondary hospital
— general practitioner with interest in diabetes
— schools representative.
Public health institutes should play key roles in providing technical support and implementing, monitoring and evaluating policy, plans and programmes relating to NCD prevention and control.
Key Messages
— To maintain a structured and well-organized implementation plan, it is important to have a lead agency or sector.
— Primary stakeholders or beneficiaries are those who are ultimately affected, such as the community.
— Secondary stakeholders are people or organizations involved in the implementation of the plan.
— Stakeholder engagement is an organization’s efforts to understand and involve stakeholders and their concerns in its activities and decision-making processes.
— The involvement of a broad range of stakeholders in the planning process is critical to promoting multisectoral action for NCD prevention and control.
— It is crucial to consider what type of governance mechanisms or structures will be required to ensure that the activities and objectives of the strategy can be put into practice.
— Under the coordination mechanism, a scientific committee and working group should be considered to provide advice and manage day-to-day implementation of the multisectoral action plan for NCDs.
Click here to back to main text
ACTION 2: Draw up a list of stakeholders
✤ Step 1: List potential stakeholders
— Use the collective experience of your group/team to draw up a list of potential stakeholders, their sector and their possible roles in developing an MSAP.
— Refer to Appendix 5 of the Global action plan for the prevention and control of noncommunicable diseases 2013-20 [https://apps.who.int/iris/handle/10665/94384] for guidance on which sectors to involve to address which risk factors.
— Consider those in the health sector and those outside it.
— Enter the details of potential stakeholders in Form 2.1
— Do not worry at this stage about the efficacy of these stakeholders. You will assess each stakeholder in the next MSAP development action.
ACTION 3: Assess the relative importance of stakeholders
This will enable you to assess which of the stakeholders you have identified will be of most use in the task of developing and implementing your MSAP.
✤ Step 1: Assess the potential of each stakeholder
— Review the list of potential stakeholders listed in Form 2.1 Through a group discussion assign each stakeholder a score of “low”, “medium”, or “high”, according to the group’s assessment of their capacity and resources – e.g. skills, time available, information, finances and experience.
— Enter the consensus assessment in the final column and sort the table according to that column.
— Those assessed by the majority of the group to have low capacity or resources might not be suitable for further consideration, although you should bear in mind the need to have representatives from a wide range of sectors in your team.
✤ Step 2: Assess remaining stakeholders’ effectiveness in preventing and controlling NCDs
— Focus on the stakeholders assessed as having
medium or high capacity.
Copy their names/sector/possible roles into Form
2.2
— As a group, you now need to consider their:
o role and interest in NCD prevention and control;
o level of influence; and
o the impact this may have on the NCD prevention and control programme and on other stakeholders.
— Use an analysis matrix (see Fig. A.1) in which “influence” and “importance” are the two variables used to assign each stakeholder to one of four groups. Those that fall into boxes A, B and C will be the key stakeholders of your project.
Fig.A.1 Assessment of relative importance of stakeholders importance of stakeholders
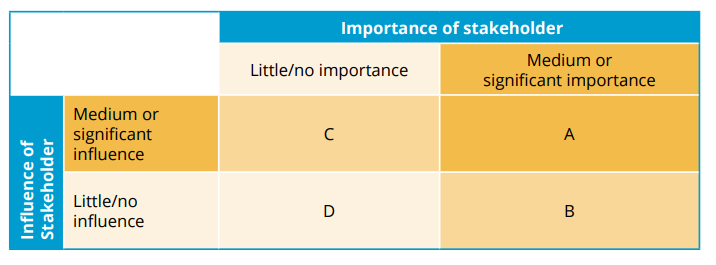
The implications of each box are summarized below:
Box A
These are stakeholders who appear to have a high degree of influence on the project and who are also of high importance for its success. This implies that the implementing organization will need to construct good working relationships with these stakeholders, to ensure an effective coalition of support for the project. Examples might be senior officials and politicians or trade unions.
Box B
These are stakeholders of high importance to the success of the project, but with low influence. This implies that special initiatives will be required to protect their interests. An example would be traditionally marginalized groups (e.g. Indigenous people, youth, seniors), who might be beneficiaries of a new service, but who have little “voice” in its development.
Box C
These are stakeholders with high influence, who can therefore affect the project outcomes but whose interests are not necessarily aligned with the overall goals of the project. They might be financial administrators who can exercise considerable discretion over funding disbursements. This conclusion implies that these stakeholders may be a source of significant risk, and they will need careful monitoring and management.
Box D
The stakeholders in this box, with low influence on, or importance to, the project objectives, are of low priority.
✤ Step 3: Enter each stakeholder’s scores in Form 2.2
ACTION 4: Engage stakeholders
Filling in Form 2.3 will help you to decide in what capacity you might engage stakeholders. This process can be used, for example, to engage stakeholders to sit on a national taskforce, a steering committee, an expert committee – at different stages in the development, implementation and evaluation of the MSAP.
✤ Step 1: Rank key priorities and define activities involved
Work with a group to make a list of key priorities for initiating the multisectoral action plan.
— Enter the priorities (including a timeframe where possible) in column 1 of Form 2.3
— In column 2 enter the activities needed to complete the action in the timeframe.
✤ Step 2: Identify potential stakeholders
— In column 3 consider the roles and responsibilities of the people needed for the activities in column 2.
— In column 4 consider which sector to turn to for stakeholders to fulfil each role.
— In column 5 ask the group for suggestions of individuals to approach.
Table A.1 includes an example priority in the first column. The questions to consider when deciding how to engage with stakeholders to fulfil the priority are listed in subsequent columns.
Table A.1 Information needed to engage stakeholders to meet a specific priority
CHECKLIST
Use the Checklist available here to make sure you have completed all the necessary steps before moving on to the next module.
- Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases (Document A/ RES/66.2). New York: United Nations; 2011 (A/RES/66/2;https://digitallibrary.un.org/record/720106,accessed 1 November 2021).
- Global action plan for the prevention and control of NCDs 2013–2020. Geneva: World Health Organization; 2013 (https://apps.who.int/iris/handle/10665/94384,accessed 1 November 2021) .
- Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014 (http://apps.who.int/iris/handle/10665/148114,accessed 1 November 2021).
-
Citation
World Health Organization.(2022). Toolkit for developing a multisectoral action plan for noncommunicable diseases: module 2: establishing stakeholder engagement and governance mechanisms. World Health Organization. https://apps.who.int/iris/handle/10665/353159 . License: CC BY-NC-SA 3.0 IGO.
ISBN of Module 2 is -
9789240043510 (electronic version)
9789240043527 (print version)
- FAO, WHO (2014). Rome declaration on nutrition. Rome: Food and Agriculture Organization of the United Nations (https://www.fao.org/3/ml542e/ml542e.pdf)
- UN (2011). Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations (A/RES/66/2; https://digitallibrary.un.org/record/710899/?ln=en) .
- WHO. Global health estimates [online database]. Geneva: World Health Organization ( https://www.who.int/data/global-health-estimates)
- WHO. Global Health Observatory (GHO) [online database]. Noncommunicable diseases: risk factors. Geneva: World Health Organization (https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/ncd-risk-factors)
- WHO. Global targets tracking tool [online resource]. Geneva: World Health Organization (https://www.who.int/tools/global-targets-tracking-tool)
- WHO (2006). Stop the global epidemic of chronic disease: a practical guide to successful advocacy. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/43513)
- WHO (2008). 2008–2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. Geneva: World Health Organization (https://www.who.int/nmh/publications/ncd_action_plan_en.pdf) .
- WHO (2011). Global status report on noncommunicable diseases 2010. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/44579) .
- WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/94384) .
- WHO (2014). Global status report on noncommunicable diseases. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/148114)
- WHO Regional Office for Europe (2018). Multisectoral and intersectoral action for improved health and well-being for all: mapping of the WHO European Region. Governance for a sustainable future: improving health and well-being for all: final report. Copenhagen (https://apps.who.int/iris/handle/10665/341715) .
- WHO, Finland: Ministry of Social Affairs and Health (2014). Health in all policies: Helsinki statement. Framework for country action. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/112636) .
Noncommunicable diseases (NCDs) are the leading cause of death globally, killing more people each year than all other causes combined. Contrary to common perceptions, available data show that nearly 80% of NCD-related deaths occur in low- and middle-income countries. Moreover, recent decades have witnessed a steady increase in such deaths, with vulnerable population groups often worst affected, and yet many of the dire human and social consequences could be prevented by implementing cost-effective and feasible interventions.
The Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases (2011) (1) recognizes the scale of the NCD crisis and the urgent need for action. The Global action plan for the prevention and control of NCDs 2013–2020 (2) , recently extended to 2030, provides a vision and a road map to scale up action for the prevention and control of NCDs.
The global epidemic of NCDs is widely acknowledged as a major challenge to development in the 21st century and is a significant threat to achieving the United Nations Sustainable Development Goals. In addition, globally, the main NCDs represent the greatest cause of death in people aged under 70 years, imposing years of disability on those affected and their families. The Global status report on noncommunicable diseases 2014 (3) highlights the need to intensify national multisectoral action to meet the global targets that governments have agreed upon and to protect people from cardiovascular diseases, cancers, diabetes and chronic respiratory diseases.
Countries, including some that are low-income, are showing that it is feasible to make progress and reduce premature deaths from NCDs. But that progress, particularly in low- and middle-income countries, is insufficient and uneven. The global status report of 2014 reveals a distressing gap in our ability to achieve Sustainable Development Goal target 3.4 of reducing, by one third, premature deaths from NCDs by 2030, and outlines the disparities in progress on preventing NCDs worldwide.
This toolkit is a “how to” guide for developing, implementing and evaluating a multisectoral action plan for prevention and control of NCDs. It is targeted at policy-makers, planners and programme managers, and is intended to help countries, provinces and cities meet the requirements for achieving global and national NCD targets and the Sustainable Development Goals.
The toolkit takes the user through a series of actions related to the development of a multisectoral action plan (“MSAP development actions”), and provides forms and a template framework for users to complete as they undertake these actions.
Developing a multisectoral action plan involves establishing health needs and engaging relevant stakeholders before determining the actions to take, identifying and prioritizing interventions, deciding on ways to address. NCDs while establishing support and resources for prevention and control, and evaluating progress in implementing the plan
Using the toolkit is an inclusive and participatory process that involves engaging relevant stakeholders before determining the actions to take. The toolkit focuses on the main NCDs and wider determinants of health and aims to reduce the premature mortality from NCDs and the negative impacts of these determinants on health and health inequalities.
This work entails an array of competencies, such as situation analysis, advocacy, planning, mobilizing, implementing interventions and evaluating them, and disseminating the results of the evaluation. Users can refer to programme theory and logic modelling to guide the development of their action plan. The structure of the toolkit is set out in Fig. 3.1.
Fig. 3.1 Structure of the toolkit for developing a multisectoral action plan for noncommunicable diseases
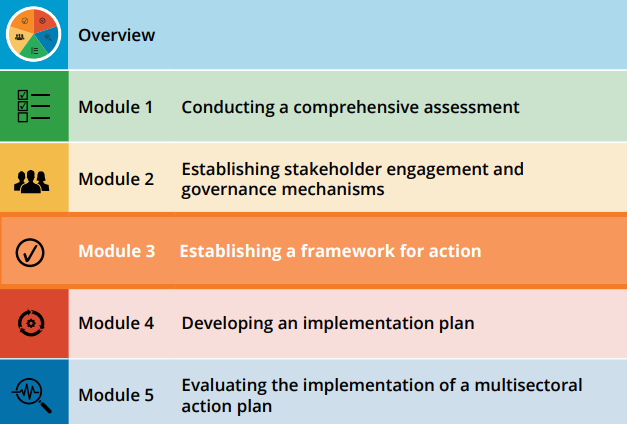
This module reframes the strategic NCD agenda by establishing an action framework for NCD prevention and control which brings together all relevant elements, including the vision, mission, and objectives, the national NCD goals and targets, the guiding principles for action, strategic areas and objectives, and the priority actions within the strategic areas.
It is important to note that guiding principles need to be agreed on by all relevant stakeholders for all NCD-related plans, irrespective of changes in goals, strategies or work approaches. This is required to ensure consistency and a joint approach to action. The Global action plan for prevention and control of noncommunicable diseases 2013–2020 (2) sets out overarching principles and approaches based on:
— human rights
— equality
— national action, international cooperation and solidarity
— multisectoral action
— life-course approach
— empowerment of people and communities
— evidence-based strategies
— universal health coverage
— management of real, perceived or potential conflicts of interest.
A framework for action provides a guide for those involved in the development of the multisectoral action plan. It starts with a wide-ranging vision and, through a series of increasingly specific intentions, brings into focus actions with measurable outcomes that can be taken to achieve that vision.
Table 3.1 summarizes the stages involved in establishing a national framework for NCD prevention and control. (The implementation of the plan and the evaluation of the process will be dealt with in modules 4 and 5 respectively.)
Table 3.1 Example of components of a framework for prevention and control of noncommunicable diseases
A vision provides an image of the future that sets expectations.
Example of a vision
All citizens live in supportive communities where they are healthy and free from preventable chronic NCDs and disabling conditions
A mission is a statement of purpose within areas of legitimate operation.
Example of a mission
To prevent noncommunicable diseases through policy changes that enable people to make healthier choices
A goal is a statement of intent or expected achievement. It refers to outcomes that are desired and achievable. The goal should be realistic and pragmatic, and at the same time reflect the main expected outcomes for NCD prevention and control.
Example of goals
— To improve the health and well-being of all people by reducing the health, social and economic impacts of NCDs
— To reduce the incidence and premature deaths attributable to NCDS
— To reduce health inequalities, including differences that occur by socioeconomic status, gender, ethnicity and location
A target is a more focused intention, typically containing a measurable outcome.
Example of targets
— 30% relative reduction in prevalence of current tobacco use by 2030
— At least 10% relative reduction in harmful use of alcohol by 2030
— 30% relative reduction in mean population intake of salt by 2030
— A 5% increase in consumption of five servings of fruit and vegetables daily by 2030
— A 10% relative reduction in prevalence of insufficient physical activity by 2030
An action plan indicator in NCD prevention and control is a number, proportion, percentage or rate that helps measure (“indicate”) the extent to which planned activities have been conducted (process and output indicators) and achievements have been made (outcome and impact indicators).
The Noncommunicable diseases global monitoring framework (4), adopted by the World Health Assembly in May 2013, includes 25 indicators and nine voluntary global targets for the prevention and control of noncommunicable diseases to be achieved by 2025. The inclusion of the targets and indicators was based on a scientific review of the current situation and trends, and a critical assessment of feasibility. Their selection was guided by several key criteria, namely public health relevance, coherence with existing strategies, an evidence-base of interventions, and feasibility of data collection and achievements of targets. The Global action plan for the prevention and control of noncommunicable diseases 2013–2020 (2) provides a roadmap that is currently being extended to 2030, for achieving the targets.
In order to measure success in meeting a target, it is necessary to establish a baseline measurement. If there are no data on which to establish such a baseline, an estimation will need to be made. However, if the indicator forms a key part of the multisectoral action plan, collecting data to establish a firm baseline should be made a priority. For instance, a measurement of salt intake cannot be a priority action if the country does not currently collect data on salt intake.
Table 3.2 provides examples of NCD targets for each of the elements listed in the Global Monitoring Framework, and baselines for those targets.
Table 3.2 Example of setting national NCD targets and establishing baselines for those targets
NCD goals, targets and indicators should be developed in collaboration with stakeholders, taking into consideration the national, regional or local context – based on a scientific review of the current situation and trends, and a critical assessment of feasibility. When setting national NCD targets, global and regional NCD targets should be considered alongside current national high-level commitments, recommendations from the situation analysis, national commitments, existing programmes, and the context of the country. A similar process should be followed when setting a provincial or city target.
MSAP DEVELOPMENT ACTION 5: Draw up a framework for action
A comprehensive multisectoral action plan should include a range of strategic areas of action and strategic objectives consistent with global NCD strategies, action plans, and monitoring frameworks.
Strategic action areas
Selecting strategic action areas is key to achieving NCD goals and targets. The following strategic areas and their key components were identified in the Global strategy for the prevention and control of noncommunicable disease (5) and the Global action plan for prevention and control of noncommunicable diseases 2013–2020 (2):
— Governance for NCD prevention and control, including national NCD leadership, partnership and advocacy for action, in addition to strengthening national capacity for implementation;
— Reduction of risk factors, including tobacco use, harmful use of alcohol, unhealthy diet and physical inactivity;
— Early detection and effective NCD management through strengthening of primary health care and health systems;
— Promoting high-quality NCD research; and
— Enhancing national capacity for NCD surveillance.
Strategic objectives
A strategic objective is an action-oriented statement that defines what must be done in order to achieve the strategy. Strategic objectives set the major benchmarks for success and are designed to be measurable, specific and realistic translations of the mission statement that can be used by management to guide decision-making.
Example of strategic objectives
— Strengthen national governance for NCD prevention and control
— Reduce risk factors and promote health
— Improve early detection and effective treatment of people with NCDs or at high risk through a primary care approach
— Strengthen national capacity for surveillance and monitoring
— Promote high-quality research for NCD prevention and control
Strategic objectives of the multisectoral action plan are closely aligned with the strategic action areas, and consist of a number of key components, examples of which are given in Table 3.3.
Table 3.3 Example of strategic areas and objectives, and key components
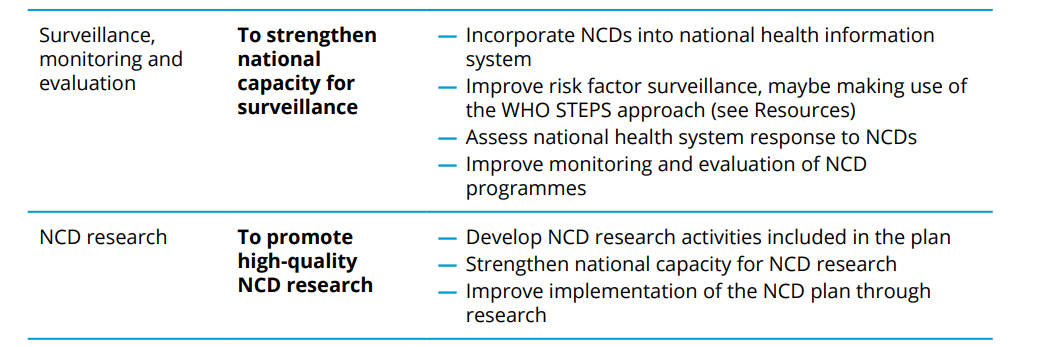
MSAP DEVELOPMENT ACTION 6: Identify strategic areas, strategic objectives and key components for your MSAP
Key Messages
— Guiding principles need to be agreed on by all relevant stakeholders for all NCD-related plans.
— A framework for action provides a guide for those involved in the development of the multisectoral action plan.
— A vision provides an image of the future.
— A mission is a statement of purpose.
— A goal refers to outcomes that are desired and achievable.
— A target contains a measurable outcome.
— An indicator measures the extent to which planned activities have been conducted and achievement have been made.
— Process and output indicators are measurements of process.
— Outcome and impact indicators are measurements of achievement.
— It is important to establish baseline data so that change can be measurable.
— The NCD Global Monitoring Framework includes 25 indicators and nine voluntary global targets for the prevention and control of noncommunicable diseases.
— Goals, targets and indicators should be developed in collaboration with stakeholders, based on a scientific review of the current situation and trends, and a critical assessment of feasibility.
— A comprehensive multisectoral action plan should include a range of strategic areas and strategic objectives that are consistent with the global NCD strategies, action plans, and monitoring frameworks.
— A strategic objective is an action-oriented statement that defines what must be done in order to achieve the strategy.
- Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations; 2011 (A/RES/66/2;https://digitallibrary.un.org/record/720106,accessed 1 November 2021).
- Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization; 2013 (https://apps.who.int/iris/handle/10665/94384,accessed 1 November 2021).
- Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014 (http://apps.who.int/iris/handle/10665/148114,accessed 1 November 2021).
- NCD global monitoring framework. Geneva: World Health Organization; 2013 (https://www.who.int/teams/ncds/surveillance/monitoring-capacity/gmf).
- WHO (2000). Global strategy for the prevention and control of noncommunicable diseases. Report by the Director-General. Geneva, World Health Organization (A53/14; https://apps.who.int/gb/ebwha/pdf_files/WHA53/ea14.pdf).
-
Citation
World Health Organization. (2022). Toolkit for developing a multisectoral action plan for noncommunicable diseases: module 3: establishing a framework for action. World Health Organization. https://apps.who.int/iris/handle/10665/353161 . License: CC BY-NC-SA 3.0 IGO.
ISBN of Module 3 is -
9789240043534 (electronic version)
97892400043541 (print version)
- Commission on Macroeconomics and Health (2001). Macroeconomics and health: investing in health for economic development. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/42463).
- Commission on Social Determinants of Health (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Final report: executive summary. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/69832).
- FAO, WHO (2014). Rome declaration on nutrition. Rome: Food and Agriculture Organization of the United Nations (https://www.fao.org/3/ml542e/ml542e.pdf).
- McQueen DV, Wismar M, Lin V, Jones CM, Davies M, editors (2012). Intersectoral governance for health in all policies: structures, actions and experiences. Copenhagen: WHO Regional Office for Europe, on behalf of the European Observatory on Health Systems Policies (https://www.euro.who.int/__data/assets/pdf_file/0005/171707/Intersectoral-governance-for-health-in-all-policies.pdf).
- UN (2014). Outcome document of the high-level meeting of the General Assembly on the comprehensive review and assessment of the progress achieved in the prevention and control of non-communicable diseases. New York: United Nations (A/RES/68/300; https://research.un.org/en/docs/ga/quick/).
- WHO. Global targets tracking tool [online resource]. Geneva: World Health Organization (https://www.who.int/tools/global-targets-tracking-tool).
- WHO. NCD global monitoring framework [website]. Geneva: World Health Organization (https://www.who.int/teams/ncds/surveillance/monitoring-capacity/gmf,accessed 1 November 2021).
- WHO. STEPwise approach to NCD risk factor surveillance (STEPS) [Online tool] Geneva: World Health Organization (https://www.who.int/teams/noncommunicable-diseases/surveillance systems-tools/steps).
- WHO (2000). Global strategy for the prevention and control of noncommunicable diseases. Report by the Director-General. Geneva, World Health Organization (A53/14;https://apps.who.int/gb/ebwha/pdf_files/WHA53/ea14.pdf).
- WHO (2004). Resolution WHA57.17. Global strategy on diet, physical activity and health. In: Fifty-seventh World Health Assembly, Geneva, 17–22 May 2004. Resolutions and decisions, annexes. Geneva: World Health Organization:31–49 (WHA57/2004/REC/1; (https://apps.who.int/gb/ebwha/pdf_files/WHA57/A57_REC1-en.pdf).
- WHO (2006). Stop the global epidemic of chronic disease: a practical guide to successful advocacy. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/43513).
- WHO (2008). 2008–2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/44009/).
- WHO (2010). Resolution WHA63.13. Global strategy to reduce the harmful use of alcohol. In: Sixty-third World Health Assembly, Geneva, 17–21 May 2010. Resolutions and decisions, annexes. Geneva: World Health Organization:23–24 (WHA63/2010/REC/1;(https://apps.who.int/gb/ebwha/pdf_files/WHA63-REC1/WHA63_REC1-en.pdf).
- WHO (2011). Global status report on noncommunicable diseases 2010. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/44579).
- WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/94384).
- WHO (2013). Resolution WHA66/10. Follow-up to the political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. In: Sixty-sixth World Health Assembly, Geneva, 20–27 May 2013. Resolutions and decisions, annexes. Geneva: World Health Organization; 2013:16–21 (WHA66/2013/REC/1;https://apps.who.int/gb/ebwha/pdf_files/WHA66-REC1/A66_REC1-en.pdf).
- WHO (2014). Global status report on noncommunicable diseases 2014. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/148114).
- WHO (2014). Noncommunicable diseases global monitoring framework: indicator definitions and specifications. Geneva: World Health Organization (https://www.who.int/teams/ncds/surveillance/monitoring-capacity/gmf, accessed 4 November 2021).
- WHO (2019). Global health estimates [online database]. Geneva: World Health Organization (https://www.who.int/data/global-health-estimates).
- WHO (2019). Global Health Observatory (GHO) [online database]. Noncommunicable diseases: risk factors. Geneva: World Health Organization (https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/ncd-risk-factors).
- WHO Regional Office for Europe (2018). Multisectoral and intersectoral action for improved health and well-being for all: mapping of the WHO European Region. Governance for a sustainable future: improving health and well-being for all: final report. Copenhagen (https://apps.who.int/iris/handle/10665/341715).
- WHO, Finland: Ministry of Social Affairs and Health (2014). Health in all policies: Helsinki statement. Framework for country action. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/112636).
- Allen LN, Smith RW, Simmons-Jones F, Roberts N, Honney R, Currie J (2020). Addressing social determinants of noncommunicable diseases in primary care: a systematic review. Bull World Health Organ. 98(11):754-65B. doi: 10.2471/blt.19.248278.
- Shao R, Feil C, Wild CK, Morschel K, Bonyani A, Smith R et al (2021). Assessing the characteristics of 110 low- and middle-income countries’ noncommunicable disease national action plans. Int J Noncommun Dis. 6(2):56-71.
- Tuangratananon T, Wangmo S, Widanapathirana N, Pongutta S, Viriyathorn S, Patcharanarumol W, et al (2019). Implementation of national action plans on noncommunicable diseases, Bhutan, Cambodia, Indonesia, Philippines, Sri Lanka, Thailand and Viet Nam. Bull World Health Organ. 97(2):129.
- Wickramasinghe K, Wilkins E, Foster C, Fadhil I, Hammerich A, Slama S et al (2018). The development of national multisectoral action plans for the prevention and control of noncommunicable diseases: experiences of national-level stakeholders in four countries. Glob Health Action. 11(1):1532632. doi: 10.1080/16549716.2018.1532632.
Click here to back to main text
ACTION 5: Draw up a framework for action
✤ Step 1: Establish a subgroup of stakeholders to collaborate on setting NCD goals, targets and indicators
From the stakeholder group already established while working on Module 2, bring together a subgroup to set NCD goals, targets and indicators.
✤ Step 2: Share information relating to national and international NCD targets and SDG target 3.4 with the group
— See the Resources section.
✤ Step 3: Vision
— Use a collective decision-making process to arrive at a Vision for your framework for action.
— Enter it in the appropriate cell in the MSAP template.
✤ Step 4: Mission
— Use a collective decision-making process to arrive at a Mission for your action framework.
— Enter it in the appropriate cell in the MSAP template.
✤ Step 5: Goal
— Use a collective decision-making process to arrive at a Goal for your action framework.
— Enter it in the appropriate cell in the MSAP template.
✤ Step 7: Baselines and targets
— Download the Noncommunicable diseases global monitoring framework:indicator definitions and specifications [https://www.who.int/teams/ncds/surveillance/monitoring-capacity/gmf], and use it as a guide to writing your baselines and targets.
— Research the baseline relevant to your country/province/city for each of the Global Monitoring Framework (GMF) elements listed on Form 3.1 and fill it in.
— Discuss with the group a suitable target for each of the GMF elements, referring to the situation analysis carried out and summarized in ACTION 1, and aligning the NCD targets with SDG target 3.4. (When planning the implementation of your MSAP in Module 4 you will be invited to prioritize some of these targets.) Enter the results of the discussion in Form 3.1
— After the meeting, copy the agreed information into the MSAP template.
ACTION 6: Identify strategic action areas and objectives
and key components
✤ Step 1: Set strategic objectives
✤ Step 1: Set strategic objectives
— Work with your group to establish a strategic objective in each of the areas listed in Form 3.2 Setting strategic objectives and key components.
— You may find it helpful to refer to two documents listed in the Resources section of this module: WHO (2008) 2008–2013 Action plan for the global strategy for prevention and control of noncommunicable disease and WHO (2013) Global action plan for prevention and control of noncommunicable diseases 2013–2020.
✤ Step 2: Itemise key components
Work with your group to establish the key components of each strategic objective.
✤ Step 3: Enter the results of the discussions in the MSAP template
This will complete the framework of your multisectoral action plan. In Module 4 you will develop an implementation plan.
CHECKLIST
Use the Checklist available here to make sure you have completed all the necessary steps before moving on to the next module.
Example of goals
- To improve the health and well-being of all people by reducing the health, social and economic impacts of NCDs.
- To reduce the incidence and premature deaths attributable to NCDs.
- To reduce health inequalities, including differences that occur by socioeconomic status, gender, ethnicity and location.
The NCD Global Monitoring Framework adopted by the World Health Assembly in May 2013 includes 25 indicators and 9 voluntary global targets for the prevention and control of noncommunicable diseases to be achieved by 2025. The inclusion of the targets and indicators was based on a scientific review of the current situation and trends, and critical assessment of feasibility. Their selection was guided by several key criteria, namely public health relevance, coherence with existing strategies, an evidence-base of interventions, and feasibility of data collection and achievements of targets. The WHO Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020 (NCD GAP) (see “Tools, resources and links” below) provides a road MSAP for achieving the targets.
Member States are encouraged to consider the development of national NCD goals and targets building on the global NCD targets and framework, may choose to consider expanding upon the core set to assure coverage of geographic priorities and key subpopulation monitoring. Targets should be relevant to the national burden of NCDs, and attainable. They might be more or less ambitious than the global targets, depending on the country context. Achievement of these targets should represent major progress in reducing NCDs and their risk factors. The template provides the methods for setting national targets.
Examples of targets
- 30% reduction in prevalence of current tobacco smoking by 2030;
- At least 10% relative reduction in overall alcohol consumption by 2030;
- 30% relative reduction in mean population intake of salt by 2030;
- Increase daily consumption of 5 servings of fruits and vegetables from 5%
- Increase daily consumption of 5 servings of fruits and vegetables from 5%; • 20% relative reduction in prevalence of insufficient physical activity by 2030.
Examples of objectives
- To strengthen national governance for NCD prevention and control
- To reduce risk factors and promote health
- To improve early detection and effective treatment of people with NCDs or at high risk through a primary care approach
- To strengthen national capacity for surveillance and monitoring
- To promote high quality research for NCD prevention and control
Selecting strategic action areas are key to achieving NCD goals and targets. The following key areas were identified in the WHO global strategy for prevention and control of noncommunicable disease, global NCD action plan 2013-20, and WHO EB134/14 documents.
Strategic objectives for NCD prevention and control are long-term national goals that help to convert a mission statement from a broad vision into more specific plans. They set the major benchmarks for success and are designed to be measurable, specific and realistic translations of the mission statement that can be used by management to guide decision-making. The box below provides a few examples of NCD MSAP’s strategic objectives.
Priority-setting of NCD interventions is needed to maximize impact where health budgets are limited and the funding of every intervention unfeasible. Prioritization allows the use of available resources – health budget, workforce, time, equipment and infrastructure – for interventions which are most likely to reach NCD targets, and to address the most important issues and needs.
The WHO website provides further guidance and methods to set national NCD targets and indicators:
Tools:
Joint Assessment of National Health Strategies (JANS) Tool & Guidelines
WHO tools to prevent and control noncommunicable diseases
Links to the tools by targets
Target 1: Reduce mortality from NCDs
Target 2: Reduce harmful use of alcohol
Target 3: Reduce prevalence of physical inactivity
Target 6: Reduce prevalence of raised blood pressure
Target 7: Halt the rise in diabetes and obesity
Target 8: Provide drug therapy to prevent heart diseases
Target 9: Provide essential medicines to treat NCDs
Links to the tools by objectives
Objective 2: Strengthen national capacity
Objective 3: Reduce risk factors
Objective 4: Strengthen health systems
WHO NCD Global Monitoring Framework
WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–20
WHO Global Nutrition Targets 2025
WHO (2011). Scaling up action against noncommunicable diseases: How much will it cost?
Noncommunicable diseases (NCDs) are the leading cause of death globally, killing more people each year than all other causes combined. Contrary to common perceptions, available data show that nearly 80% of NCD-related deaths occur in low- and middle-income countries. Moreover, recent decades have witnessed a steady increase in such deaths, with vulnerable population groups often worst affected, and yet many of the dire human and social consequences could be prevented by implementing cost-effective and feasible interventions.
The Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases (2011) (1) recognizes the scale of the NCD crisis and the urgent need for action. The Global action plan for the prevention and control of NCDs 2013–2020 (2) , recently extended to 2030, provides a vision and a road map to scale up action for the prevention and control of NCDs.
The global epidemic of NCDs is widely acknowledged as a major challenge to development in the 21st century and is a significant threat to achieving the United Nations Sustainable Development Goals. In addition, globally, the main NCDs represent the greatest cause of death in people aged under 70 years, imposing years of disability on those affected and their families. The Global status report on noncommunicable diseases 2014 (3) highlights the need to intensify national multisectoral action to meet the global targets that governments have agreed upon and to protect people from cardiovascular diseases, cancers, diabetes and chronic respiratory diseases.
Countries, including some that are low-income, are showing that it is feasible to make progress and reduce premature deaths from NCDs.But that progress, particularly in low- and middle-income countries, is insufficient and uneven. The global status report of 2014 reveals a distressing gap in our ability to achieve Sustainable Development Goal target 3.4 of reducing, by one third, premature deaths from NCDs by 2030,and outlines the disparities in progress on preventing NCDs worldwide.
This toolkit is a “how to” guide for developing, implementing and evaluating a multisectoral action plan for prevention and control of NCDs. It is targeted at policy-makers, planners and programme managers, and is intended to help countries, provinces and cities meet the requirements for achieving global and national NCD targets and the Sustainable Development Goals.
The toolkit takes the user through a series of actions related to the development of a multisectoral action plan (“MSAP development actions”), and provides forms and a template framework for users to complete as they undertake these actions.
Developing a multisectoral action plan involves establishing health needs and engaging relevant stakeholders before determining the actions to take, identifying and prioritizing interventions, deciding on ways to address NCDs while establishing support and resources for prevention and control, and evaluating progress in implementing the plan
Using the toolkit is an inclusive and participatory process that involves engaging relevant stakeholders before determining the actions to take. The toolkit focuses on the main NCDs and wider determinants of health and aims to reduce the premature mortality from NCDs and the negative impacts of these determinants on health and health inequalities.
This work entails an array of competencies, such as situation analysis, advocacy, planning, mobilizing, implementing interventions and evaluating them, and disseminating the results of the evaluation. Users can refer to programme theory and logic modelling to guide the development of their action plan. The structure of the toolkit is set out in Fig. 4.1.
Fig. 4.1 Structure of the toolkit for developing a multisectoral action plan for noncommunicable diseases
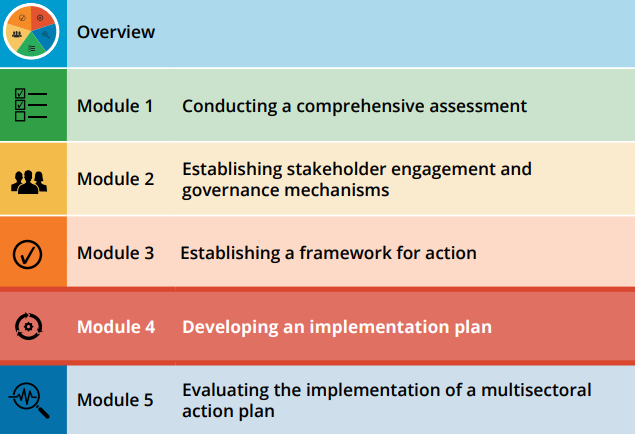
This module provides guidance on implementing the multisectoral action plan. An implementation plan is developed by a team, using multi-voting and scoring techniques to arrive at a series of priority interventions. An implementation matrix is developed, detailing how the priority interventions are to be achieved: activities, responsible leads and the timeframes they are working within, milestones and outputs to be attained, and the indicators with which to measure attainment. A costing sheet is provided for detailing the resources required. The user is also encouraged to develop strategies for implementation.
When considering a multisectoral action plan (MSAP), it is important to take into account various issues relating to its implementation. Implementation is defined as a specified set of activities designed to put into practice an activity or programme. Implementation measures therefore need to be purposeful, and to be described in sufficient detail that independent observers can detect the presence and strength of the specific set of activities related to implementation.
This information can be developed through an implementation matrix – a form on which the elements of the plan, arrived at through the various development actions provided in the module, can be recorded. Activities and a timeframe for each intervention can be decided upon and recorded, along with which agency will be responsible for the activities, the expected milestones/outputs, resources required (if possible), and the indicators needed to monitor progress. See Annex B for an example implementation plan matrix.
The information in the matrix can subsequently be used to build the Implementation Plan section of the MSAP template.
The strategic objectives of the multisectoral action plan for NCDs were established in Module 3 and entered into the Framework of the MSAP template. These now form the basis of the implementation plan.
MSAP DEVELOPMENT ACTION 8: Initiate the development of the implementation plan
Meeting the strategic objectives and the NCD targets will involve a series of interventions. The Updated Appendix 3 of the Global action plan for prevention and control of noncommunicable diseases (4) offers a list of cost-effective interventions – so-called “best-buys” – and policy options to tackle NCDs and their risk factors. These can be used as a reference at different stages of the development of the multisectoral action plan, from assessment and engagement through to the setting of a strategic NCD agenda and an implementation plan.
Framing priorities
It is important to make interventions as specific as possible. Broad aims and statements that fail to consider the practical implications (such as “reduce physical inactivity”) make it difficult to assess for effectiveness and feasibility.
Examples of interventions with specific directions are:
— Adopt and implement national guidelines on physical activity for health.
— Create and preserve built and natural environments that support physical activity in key settings with a particular focus on providing infrastructure to support active transport – i.e. walking and cycling – active recreation and play, and participation in sports.
— Train primary health care professionals to encourage exercise and physical activity uptake.
Ensuring that specific and comprehensive interventions that address population, community and individual health determinants are included at this stage is essential for the success of the prioritization process and the resulting action plan. The responsible officer needs to identify specific, implementable interventions prior to the prioritization process.
Three main factors need to be considered when drawing up interventions:
1. Are existing interventions already being implemented? If there are active interventions addressing the health target, it is important to include these in the menu as policy options and interventions so they can also be included in the prioritization process and considered for ongoing support.
2. Do all stakeholders participating in the prioritization process understand the proposed interventions? For example, does everyone understand what the intervention “implement effective drink-driving policies and countermeasures” entails? If they do, then it may not be necessary to substantiate the intervention with directly actionable activities (e.g. lowering the legally permissible blood alcohol level, increasing fines for drunk driving etc.). However, if they do not, these will need to be developed in order to score them later for feasibility and effectiveness. To identify directly actionable activities, Member States may refer to regional and global WHO strategies and guidance. Working with topic experts from the ministry of health and professional organizations to obtain their input on suitable interventions is also advisable.
3. Can interventions be implemented independently, or do they need to be implemented as a package? For example, can the intervention “increase consumption of fruits and vegetables” be implemented simultaneously? Or is it possible to address fruit consumption and vegetable consumption separately, in a staggered approach, and still have a positive impact on the population’s total fruit and vegetable consumption? If the former, it is advisable to identify specific interventions as part of the action plan. If the latter, it is recommended to identify specific actions before prioritization in order to score them for feasibility and effectiveness.
All interventions suggested to achieve NCD targets should be as specific as possible and fulfil the following requirements:
— Respond to the situation analysis.
— Demonstrate a quantifiable effect size, as evidenced by at least one peer-reviewed, published study.
— Possess a clear link to the outcome described by the vision and goals.
— Possess a clear link to national NCD targets.
MSAP DEVELOPMENT ACTION 9: List possible interventions for each strategic objective
Where health budgets are limited and it is not feasible to fund every intervention, it will most likely be necessary to prioritize NCD interventions in order to maximize impact. Prioritization allows the use of available resources – health budgets, workforce, time, equipment and infrastructure – for interventions that are most likely to reach NCD targets, and to address the most important issues and needs.
Selecting methods and approaches to setting priorities
A participatory approach to prioritization is recommended, bringing together all relevant stakeholders in workshops, group discussions or online forums.
Workshops
Workshops bring together all relevant stakeholders in a communal setting. The workshop setting allows comprehensive sharing of information, builds transparency, fosters inclusion, and allows stakeholders to raise ideas and concerns to enhance consensus.
In order to address each of the strategic objectives and prioritize the possible interventions, a number of workshops may be necessary. The workshops should be conducted over as short a time span as possible (ideally within 1 to 2 months).
Web-based techniques
Where key stakeholders are unable to attend a workshop or group discussion in person, the process outlined in Actions 10 and 11 can be replicated online through web-based platforms. Stakeholders can complete the steps of the prioritization process through shared spreadsheets or online questionnaires. It is recommended that the facilitator establishes an online forum to enable stakeholders to raise queries or concerns throughout the process and to update them on the results.
An important part of the development of any action plan is the identification of policy options and effective and cost-effective interventions to meet the NCD targets included in the Framework drawn up in Module 3. (Note that throughout this toolkit the term “intervention” is inclusive of all strategies, policies and programmes that improve mental and physical health, or discourage or reframe those with health risks for individuals and populations.)
The process of prioritizing interventions (Fig. 4.2) starts with an overview of the findings of the situation analysis conducted in Module 1, in relation to the objectives and the proposed interventions. All stakeholders should agree on the approaches, methods and basic criteria for determining priorities or focusing areas for action. Multi-voting and scoring methods should then be used to narrow down and rank the interventions. The final outcome of the prioritization process is a ranked list of interventions which stakeholders agree are most relevant to achieving the respective objective.
Fig. 4.2 The step-by-step process for prioritizing policy options and interventions
A menu of potential policy options and interventions to achieve the respective objectives and targets should be established, based on the situation analysis. It is recommended that the description of policy options includes specific actions and policy-based interventions to ensure that they will be effective in meeting NCD targets. They should cover crucial interventions at the population level (e.g. policies, regulations, guidelines), at the community level (e.g. settings-based programmes, social marketing, education) and at the individual level (e.g. health services and medical interventions) to address the NCD targets.
Population-wide interventions. A number of interventions to prevent NCDs on a population-wide basis are highly cost-effective as well as being inexpensive, feasible and culturally acceptable to implement. Other population-wide interventions are cost-effective and low cost, while still others have strong evidence though they currently lack research on their cost-effectiveness.
Individual health-care interventions. These are interventions for individuals who either already have NCDs or who are at high risk of developing them. Evidence shows that such interventions can be very effective and are usually cost-effective or low in cost. For example, highrisk individuals and those with established cardiovascular disease can be treated with regimens of low-cost generic medicines that significantly reduce the likelihood of death or of vascular events.
When combined, population-wide and individual interventions may save millions of lives and considerably reduce human suffering from NCDs. The WHO Global status report on noncommunicable diseases 2014 (3) examines existing interventions and identifies some as “best buys”. These are high impact and highly cost-effective, and also inexpensive, feasible and culturally acceptable to implement – even in resource-constrained settings.
Tobacco
— Reduce affordability of tobacco products by increasing tobacco excise taxes.
— Create, by law, completely smoke-free environments in all indoor workplaces, public places and public transport.
— Warn people of the dangers of tobacco and tobacco smoke through effective health warnings and mass media campaigns.
— Ban all forms of tobacco advertising, promotion and sponsorship.
Harmful use of alcohol
— Regulate commercial and public availability of alcohol.
— Restrict or ban alcohol advertising and promotions.
— Use pricing policies such as excise tax increases on alcoholic beverages.
Diet and physical activity
— Reduce salt intake.
— Replace trans fats with unsaturated fats.
— Implement public awareness programmes on diet and physical activity.
— Promote and protect breastfeeding.
Cardiovascular disease and diabetes
— Provide drug therapy (including glycaemic control for diabetes mellitus and control of hypertension using a total risk approach) and counselling to individuals who have had a heart attack or stroke and to persons with high risk (≥30%) of a fatal and nonfatal cardiovascular event in the next 10 years.
— Prescribe acetylsalicylic acid (aspirin) for acute myocardial infarction Cancer.
Cancer
— Reduce risk of liver cancer through hepatitis B immunization.
— Reduce risk of cervical cancer through screening (visual inspection with acetic acid (VIA) linked with timely treatment of pre-cancerous lesions).
A further list of policy recommendations for NCD prevention and control, including the “best-buys” and “good-buys”, is contained in Appendix 3 of the Global action plan for the prevention and control of NCDs (2) and in the Updated Appendix 3 of 2017 (4).
MSAP DEVELOPMENT ACTION 10: Narrow down interventions for further assessment
Once the list of possible interventions for inclusion in the plan has been narrowed down, based on the expertise and experience of the stakeholder group, the interventions need to be assessed in terms of effectiveness and feasibility. As far as possible, interventions should be judged against these two criteria based on quantitative country data. In the absence of such data, reference can be made to the website WHO Cost effectiveness and strategic planning (WHO-CHOICE) (5) , which contains data on the costeffectiveness of interventions, and country-specific information on many health topics. If the required data are not available, qualitative judgements will have to be made in lieu of available country statistics.
Additional criteria can be used to prioritize interventions so that considerations specific to the political or economic context or cultural background of a Member State are included (see Table 4.1). Additional criteria should receive buy-in by all core stakeholders and be appropriate to the country situation. Ideally, there should be recognized prioritization criteria, as evidenced by at least one published, peer-reviewed article.
Table 4.1 A list of possible criteria to be used in addition to feasibility and effectiveness
MSAP DEVELOPMENT ACTION 11:Assess interventions in terms of effectiveness and feasibility
The priority interventions arrived at through a series of workshops in MSAP DEVELOPMENT ACTION 11 will need to be screened by smaller working groups of core stakeholders to produce a final list of comprehensive and cohesive interventions that fits with policies, agendas and available resources.
The list of interventions needs to assist the Member State, province or city to meet its health targets by addressing the three levels of healthcare:
1. Interventions aimed at the whole population taking a national approach;
2. Interventions aimed at the whole population taking a community approach; and
3. Interventions at an individual or clinical level.
To maintain a structured and well-organized implementation plan, a lead agency or sector should be identified on the plan. The ministry of health or similar authority in government is critical in facilitating development and implementation of the multisectoral action plan. The ministry of health can facilitate multisectoral action through:
— coordinating multiple agencies;
— engaging relevant sectors and optimizing meaningful participation;
— organizing committee meetings;
— following up on decisions made by the coordinating bodies;
— identifying implementation gaps and proposing measures to implement new strategies; and
— preparing consolidated reports.
A timeframe should be specified in the implementation plan, including expected start and end dates. Some programmes last for a few months, while others may become regular parts of health systems.
Timelines allow for monitoring and management of the plan's implementation. While timelines may be adjusted as the implementation progresses, it is always good practice to specify timelines as an integral part of the planning process, so that stakeholders are aware of what is expected of them.
Milestones
A milestone is a marker in a plan that signifies a change or stage in the implementation. Milestones are powerful components in plans and project management, because they show key events and forward movement. Milestones should be given for each key activity to ensure that all stakeholders are aware of the schedule and completion dates for projects. Examples of milestones that programme managers might include in their multisectoral action plan for NCDs are:
— start and end dates for the plan
— key deliveries
— stakeholder approvals
— validation of the plan
— important meetings and presentations.
Outputs
Outputs of an action plan are accomplishments, products or activities – such as workshops, meetings, counselling, training, publication, recruitment and media work – intended to lead to an outcome.
Example outputs of a national action plan:
— national partnership for NCD prevention and control established
— a number of national NCD programmes developed
— annual meetings with relevant stakeholders held
— a number of workshops organized, and a number of health professionals trained
— materials on healthy diet, physical activity, tobacco use developed.
The implementation plan is a management tool and must be revisited regularly to determine the progress of the interventions. Indicators specify how progress can be monitored and measured and will inform decisions about whether the desired outcomes have been achieved. Examples of indicators are:
— age-standardized mean population intake of salt (sodium chloride) per day in grams in persons aged 18+ years
— age-standardized prevalence of overweight and obesity in persons aged 18+ years (defined as body mass index greater than 25 kg/m² for overweight or 30 kg/m² for obesity)
— number of sedentary adults
— number of adults who practise moderate physical activity on a daily basis
— number of adolescents who practise moderate physical activity five days a week.
Integrating NCD monitoring into public health infrastructure
NCD surveillance and monitoring systems are essential components of a health information system. This is all the more important where resources are limited. This aim can be supported by:
— using existing information systems so that national NCD surveillance and monitoring systems build upon a country's existing information infrastructure;
— utilizing local resources to build a surveillance and monitoring culture;
— maintaining an ongoing surveillance and monitoring programme;
— incorporating NCD surveillance and monitoring into national health information systems; and
— supporting innovation in data collection technology.
For countries with little existing NCD surveillance and monitoring, the development of a system should be incremental. In settings with limited capacity, a viable and sustainable system needs to be simple and to begin by producing data at a local level. Enhancing the quality of existingsurveillance and monitoring should take priority over expansion of a poor system.
MSAP DEVELOPMENT ACTION 12:Develop details of priority interventions
A cost estimate for the multisectoral action plan will involve breaking down the total budget (identified at the outset of the planning process) into its component values.
The process will involve consideration of all actions related to the implementation of the priority interventions and the total cost for every year of implementation, using all available information. Different cost scenarios should be considered for the implementation of the plan at national, regional and local levels. The timeframe and scope of the activities involved may need to be adjusted to fit with available resources.
An example of a costing sheet (without figures) is provided in Table 4.1.
Table 4.1 Example costing sheet
MSAP DEVELOPMENT ACTION 13: Create a costing sheet for the implementation of the MSAP and summary
For a multisectoral action plan to be successfully implemented, a good strategy will take into account existing barriers and resources (people, funding, materials, etc.). It will also follow the overall vision, mission, and objectives of the MSAP Framework.
A multisectoral action plan for NCDs will use many different strategies: providing information, strengthening collaboration with relevant sectors, enhancing support, strengthening organizational and health providers’ capacity, removing barriers, providing resources to achieve its goals. The following are examples of implementation strategies:
— Advocate for public action (e.g. develop appropriate key messages targeting high-risk population);
— Develop health policies to support the implementation of the plan (e.g. convene policy dialogue with stakeholders to get consensus on health policy for NCD prevention and control);
— Engage relevant sectors involved in NCD prevention and control (e.g.establishment of multisectoral coordination);
— Strengthen health systems that provide services for people with, or at risk of developing, NCDs (e.g. increase the number of public health centres that provide health care, increase essential NCD medicine);
— Improve the capacity of health care providers (e.g. provide training programmes in order to provide specific services for people with, or at risk of developing, an NCD);
— Promote behavioural changes (e.g. engage the target audience for the intervention in order to understand the behaviour and factors influencing it from their perspective);
— Modify barriers, access, exposures, and opportunities (e.g. build healthy environments to reduce resistance of patients to changing risky behaviour;
— Provide information and enhance skills (e.g. conduct a social marketing campaign to educate people about the problem or goal and how to address it);
— Involve community sectors (e.g., mobilize people to prepare healthy food through community committees);
— Implement the interventions (e.g. pilot the interventions and continuously monitor them to provide guidance for adapting interventions to achieve a good fit between the interventions and context); and
— Improve implementation of the technical guidelines (e.g. establish supervision mechanism).
For a multisectoral action plan to be successful, it is necessary to devise implementation strategies to gain and maintain support for it. The most suitable mechanisms for coordinating multisectoral actions will depend on the context. There are a variety of approaches to national coordination (see Module 2, Section 2 Establishing a governance mechanism). These include:
— national NCD committees, councils, or steering committees
— working groups or executive committees
— scientific committees
— provincial or local coordination mechanisms.
MSAP DEVELOPMENT ACTION 14:Develop implementation strategies
Although the approval process will vary, it is essential that NCD prevention and control plans are approved or endorsed at the highest level possible to ensure continued political support.
After the multisectoral action plan for NCDs is approved, it is important that it is disseminated and communicated by the ministry of health to key players and the public, to raise awareness and support. Many policies fail to be implemented because they are poorly communicated.
Dialogue and debate through social media can be an effective way of raising public awareness and maintaining national interest in NCD prevention and control. Facilitating public discourse and disseminating information on the social and economic costs of NCDs on individuals, families and the country, can be an effective way of advocating for the resources needed.
Sources of financing for implementation of the multisectoral action plan should be identified at the outset of the development process. This finance should be sufficient to cover the cost of all priority activities and the total cost for every year of implementation. Timelines and the scope of activities may need to be adjusted to fit with available resources.
The plan can be financed through a variety of innovative financing measures which might include contributions from sustainable domestic, multilateral and bilateral funding initiatives.
In order to get specific annual budgetary allocation at governorate levels, the following questions should be asked:
— Are there adequate, predictable and sustainable financing mechanisms and resources for undertaking the activities and the provision of health services?
— Are there current financing models that could fund the action plan – or what new ones could be found, if needed?
— Are there financial risks to implementing anticipated activities?
— Are there innovative approaches to funding (e.g. funds can come from tobacco and soft drink taxation for NCD prevention and control or issuing of government bonds or diaspora bonds)?
— Are there attractive sustainable donor investments or collaboration with NGOs, international organisations and/or other large non-state actors?
Key Messages
— Implementation measures need to be purposeful and their results detectable.
— It is necessary to prioritize interventions, especially where health resources are limited.
— Interventions need to be specific and implementable.
— A participatory approach to prioritization is recommended, bringing together all relevant stakeholders, either in person or online.
— A lead agency should be identified.
— It is important to set a timeframe for the plan and specify timelines for actions.
— Milestones are markers that signify a stage in the implementation.
— Outputs are planned activities intended to lead to outcomes.
— Indicators measure whether a plan is achieving results. They specify how progress will be monitored and measured and inform decisions about success or failure.
— The costing exercise should consider the cost of activities related to implementing the priority interventions.
— A multisectoral action plan will use many different implementation strategies.
— It is essential that NCD prevention and control plans are approved or endorsed at the highest level possible to ensure continued political support.
— Sources and methods of financing the implementation of the plan need to be established early on in the planning process.
- Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations; 2011 (A/RES/66/2;https://digitallibrary.un.org/record/720106,accessed 1 November 2021).
- Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization; 2013 (https://apps.who.int/iris/handle/10665/94384,accessed 1 November 2021).
- Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014 (http://apps.who.int/iris/handle/10665/148114,accessed 1 November 2021).
- Updated Appendix 3 of the Global action plan for prevention and control of noncommunicable diseases. Technical annex. Geneva: World Health Organization; 2017 (https://www.who.int/ncds/governance/technical_annex.pdf?ua=1).
- New cost-effectiveness updates from WHO Cost effectiveness and strategic planning (WHO-CHOICE) Geneva: World Health Organization; 2021 https://www.who.int/news-room/feature-stories/detail new-cost-effectiveness-updates-from-who-choice).
-
Citation
World Health Organization. (2022). Toolkit for developing a multisectoral action plan for noncommunicable diseases: module 4: developing an implementation plan. World Health Organization. License: CC BY-NC-SA 3.0 IGO https://apps.who.int/iris/handle/10665/353160 . License: CC BY-NC-SA 3.0 IGO.
ISBN of Module 4 is -
9789240043558 (electronic version)
9789240043565 (print version)
- WHO (2012). Costing tool – user guide: scaling up action against noncommunicable diseases: how much will it cost? Geneva: World Health Organization (https://www.who.int/ncds/management/c_NCDs_costing_estimation_tool_user_manual.pdf?ua=1).
- WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/94384).
- WHO (2013). Implementation tools: package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/133525).
- WHO (2013). Resolution WHA66/10. Follow-up to the political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. In: Sixty-sixth World Health Assembly, 20–27 May 2013. Resolutions and decisions, annexes. Geneva: World Health Organization:16–20 (WHA66/2013/REC/1; https://apps.who.int/gb/ebwha/pdf_files/WHA66-REC1/A66_REC1-en.pdf).
- WHO (2014). Global status report on noncommunicable diseases 2014. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/148114).
- WHO (2015) Framework for action to implement United Nations the political declaration on the noncommunicable diseases, including indicators to assess country progress by 2018. Updated October 2015, based on resolution EM/RC59/R.2 & EM/RC60/R.4 [graphic] Geneva: World Health Organization (https://www.researchgate.net/figure/Framework-for-Action-to-Implementthe-UN-Political-Declaration-developed-by-the-WHO_fig1_324537675).
- WHO (2017). How WHO will report in 2017 to the United Nations General Assembly on the progress achieved in the implementation of commitments included in the 2011 UN political declaration and 2014 UN outcome document on NCDs. Technical Document. Geneva: World Health Organization (who.int/nmh/events/2015/Updated-WHO-Technical-Note-NCD-Progress-Monitor-September-2017.pdf?ua=1).
- WHO. Global coordination mechanism on the Prevention and Control of NCDs [website]. Geneva: World Health Organization (https://www.who.int/groups/gcm).
- WHO. OneHealth Tool [resource] (https://www.who.int/tools/onehealth,accessed 1 November 2021).
- WHO. STEPS instrument [website] Geneva: World Health Organization (https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps/instrument,accessed 1 November 2021).
- WHO (2017). Tackling NCDs: “Best buys” and other recommended interventions for the prevention and control of noncommunicable diseases. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/259232).
- WHO (2017). Updated Appendix 3 of the Global action plan for prevention and control of noncommunicable diseases. Technical annex. Geneva: World Health Organization (https://www.who.int/ncds/governance/technical_annex.pdf?ua=1) .
- WHO (2018). Noncommunicable diseases country profiles. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/274512).
- WHO (2021). New cost-effectiveness updates from WHO Cost Effectiveness and Strategic Planning (WHO-CHOICE) Geneva: World Health Organization (https://www.who.int/news-room/feature-stories/detail/new-cost-effectiveness-updates-from-who-choice, accessed 1 November 2021) .
- WHO (2021). Cancer [website] Geneva: World Health Organization (https://www.who.int/news-room/fact-sheets/detail/cancer, accessed 1 November 2021).
- WHO (2021). Cardiovascular diseases [website] Geneva: World Health Organization(https://www.who.int/news-room/factsheets/detail/cardiovascular-diseases-(cvds), accessed 1 November 2021).
- WHO (2021). Chronic obstructive pulmonary disease (COPD) [website] Geneva: World Health Organization (https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd), accessed 1 November 2021).
- WHO (2021). Diabetes [website] Geneva: World Health Organization (https://www.who.int/news-room/fact-sheets/detail/diabetes, accessed 1 November 2021) .
- WHO (2011). Global status report on noncommunicable diseases. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/44579).
- WHO (2014). Global status report on noncommunicable diseases 2014. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/148114).
- WHO (2018). Alcohol [website] Geneva: World Health Organization (https://www.who.int/news-room/fact-sheets/detail/alcohol, accessed 1 November 2021).
- WHO (2020). Physical activity [website] Geneva: World Health Organization (https://www.who.int/news-room/fact-sheets/detail/physical-activity, accessed 1 November 2021).
- WHO (2021). Malnutrition [website] Geneva: World Health Organization (https://www.who.int/news-room/fact-sheets/detail/malnutrition, accessed 1 November 2021).
- WHO (2021). Tobacco [website] Geneva: World Health Organization (https://www.who.int/news-room/fact-sheets/detail/tobacco , accessed 1 November 2021).
Policy options and cost-effective interventions
NCDs
Risk factors
- Gauri SK, Das P (2017). A framework for performance evaluation and monitoring of public health program using composite performance index. Int J Quality Res. 11:817-33. doi: 10.18421/ijqr11.04-06.
- Ghebreyesus TA (2018). Acting on NCDs: counting the cost (2018). Lancet. 391(10134):1973–4. doi: http://dx.doi.org/10.1016/S0140-6736(18)30675-5PMID:29627165
- King DK, Glasgow RE, Leeman-Castillo B (2010). Reaiming RE-AIM: Using the model to plan, implement, and evaluate the effects of environmental change approaches to enhancing population health. Am J Pub Health. 100(11):2076-84. doi: 10.2105/ ajph.2009.190959.
- Luck K, Doucet S, Luke A (2020). The development of a logic model to guide the planning and evaluation of a navigation center for children and youth with complex care needs. Child & Youth Services. 41(4):327-41. doi: 10.1080/0145935x.2019.1684192.
- Mendan S, Alwan A, editors (2011). (2011). A prioritized research agenda for prevention and control of noncommunicable diseases. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/44569 ).
- Sanni S, Wisdom JP, Ayo-Yusuf OA, Hongoro C (2019). Multi-sectoral approach to noncommunicable disease prevention policy in Sub-Saharan Africa: a conceptual framework for analysis. Int J Health Serv. 49(2):371-92. doi: 10.1177/0020731418774203.
- Shao R, Feil C, Wild CK, Morschel K, Bonyani A, Smith R et al (2021). Assessing the characteristics of 110 low- and middle-income countries’ noncommunicable disease national action plans. Int J Noncommun Dis. 6(2):56-71.
Click here to back to main text
ACTION 8: Initiate the development of an implementation plan
You will need to complete a detailed implementation plan for each of the strategic objectives you listed on your MSAP Framework.
— In preparation for this, enter the strategic objectives in the appropriate places in the Implementation Plan section of the MSAP template.
Click here to back to main text
ACTION 9: List possible interventions for each strategic objective
Refer to the Resources section, where you will find links to documents that will help you in this action.
— For each of your strategic objectives, draw up a menu of cost-effective interventions to be presented at workshops for narrowing down and prioritizing.
— Ensure that the interventions are framed in a way that will enable them to be scored for effectiveness and feasibility
— Enter the interventions in Form 4.1, creating one form for each strategic objective.
Click here to back to main text
ACTION 10: Narrow down the interventions for further assessment
The following provides a step-by-step method for a group to narrow down the list of NCD interventions. It is important to emphasize that the approach suggested is not prescriptive. It may be tailored to the specific needs of a stakeholder group or Member State.
✤ Step 1: Set criteria for prioritization
— Present the group with the lists of strategic objectives and interventions you have created using Form 4.1
— Specify, or arrive at through discussion, the number of interventions to be prioritized in Step 4.
✤ Step 2: Narrow down the interventions
If the list of potential interventions for a strategic objective exceeds the desired number, use multi-voting to narrow it down. (If not, move on to Step 4.)
— Using Form 4.1, all participants vote for all interventions they consider high priority, placing a tick against them in the column headed Round 1.
— Collect the voting forms and tally the votes. An intervention that has been voted for by fewer than half the participants is eliminated.
— If the result of Round 1 is that the desired number of interventions is reached, the voting can be stopped, but if not, continue to further rounds.
— In round 2, each stakeholder votes for the desired number of interventions. Rank each intervention according to the votes received. In the event of a tie, another round of voting on those interventions will be required to decide on which should be included.
The multi-voting technique ensures that voting is not influenced by a dominant member. Additionally, it allows interventions to make it onto a final list that are not necessarily the top priority of any participant. In contrast, a simple vote would mask the popularity of such interventions and reaching consensus would be more difficult.
Click here to back to main text
ACTION 11: Assess interventions in terms of feasibility and effectiveness
The prioritized interventions need to be scored for feasibility and effectiveness, using a multi-criteria decision analysis. Additional criteria can be used, as agreed by the stakeholders.
— Prepare copies of Form 4.2 and Form 4.3 by listing the prioritized interventions for each strategic objective.
✤ STEP 1: Score the interventions for feasibility
Provide the stakeholders with your prepared version of Form 4.2 which includes the information in Table A.1.
Table A.1: Suggested scales to score for feasibility
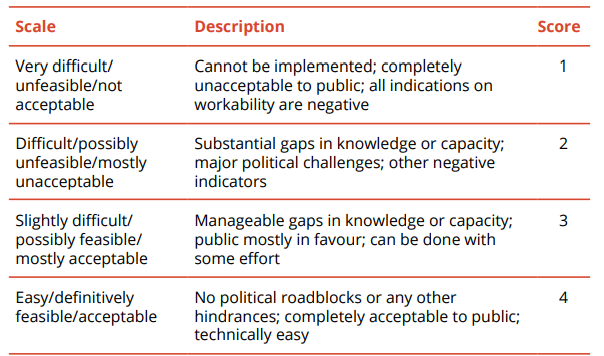
Stakeholders will be asked to give each intervention a score, depending on how easy or difficult its implementation is, based on five dimensions of feasibility:
- Technical: necessary expertise, workforce, infrastructure;
geographic
coverage; - Political: acceptability to government, political support; consistency with other policies;
- Cultural: acceptability to society and communities;
- Financial: required cost; affordability; and
- Legal: legal barriers, obligations, including trade-related commitments
— Lead a discussion on the feasibility of each intervention to allow participants to offer their viewpoints and knowledge on aspects of feasibility, and to clarify uncertainties.
— Invite participants to silently score the interventions, assigning a score for each of the five feasibility dimensions (technical, political, cultural, financial, legal).
— Ask participants to calculate the feasibility score for each intervention by adding the scores on each row and dividing them by five.
— Collect all the forms and calculate the average feasibility score for each intervention by summing each participant's total scores and dividing them by the number of participants. The higher the total feasibility score, the easier the implementation of the intervention.
✤ Step 2: Score the interventions for effectiveness
— Provide the stakeholders with your prepared version of Form 4.3 which includes the information in Table A.2.
Table A.2: Estimation of intervention effectiveness
— Lead a discussion on the effectiveness of each intervention to allow participants to offer their viewpoints and knowledge on different aspects, and to clarify uncertainties.
You may feel it appropriate to present stakeholders with background evidence on the effectiveness of the interventions, including quantitative evidence (such as cost-effectiveness analysis or DALYs (Disability Adjusted Life Years) averted per 10 million people).
Where such an analysis is not possible due to lack of available data, a stakeholders' judgements on the likelihood of an intervention being effective in addressing the health issue and the size of that effect in terms of how many people are predicted to benefit may have to be used. An estimate of how well the intervention addresses relevant risk factors, as compared with other interventions, will be relevant, alongside whether an intervention addresses more than one risk factor.
— Invite participants to silently score the interventions, assigning a score for each of the five feasibility dimensions (technical, political, cultural, financial, legal).
— Ask them to arrive at a total score by multiplying the two scores.
— Collect all the forms and calculate the average effectiveness score for each intervention by summing each participant’s total scores and dividing them by the number of participants.
✤ Step 3: Rank the interventions
Transfer the results of the assessments to Form 4.4 in order to arrive at a final ranking. Before filling in the results of Step 1, the assessment of feasibility,multiply the scores by 3 to ensure that they carry the same weight as the assessment of effectiveness.
Sum the (adjusted) score for feasibility and that for effectiveness for each intervention to establish the final score.
Use this score to rank interventions, from those judged to have the greatest impact on health outcomes to the least.
✤ Step 4: Build consensus and finalize
— Review the list of assessed interventions with the group and agree upona final list of prioritized interventions by reaching a group consensus.
Click here to back to main text
ACTION 12: Provide details of interventions
✤ Step 1: Form a small group or several groups of stakeholders to assist in translating the list of priority interventions into an implementation matrix
— Study the example of a matrix for a single objective in Annex B.
✤ Step 2: Characterize each of the prioritized interventions as core, medium-term or desirable
Through a group discussion, consider which of the following categories the interventions fit into:
— Core interventions. The initiatives that are immediately feasible and likely to have the greatest impact are selected for implementation first. It is expected that these interventions would be carried out within a twoyear timeframe.
— Medium-term interventions. These are next in terms of importance. They should be introduced as soon as possible but have a slightly lower priority than the core strategies. These interventions are feasible once there has been a realistic reallocation of resources so their start may be delayed.
— Desirable interventions. These require resources beyond the current levels, and are interventions to which the country should be aiming in the long term but are expected to have a longer timeframe (at least five years).
✤ Step 3: Enter the interventions into an implementation matrix
— On Form 4.6 fill in the objectives.
— Enter the interventions intended to meet each objective and its characterization as core, medium-term or desirable.
— Establish a realistic timeframe and enter it in the appropriate column.
✤ Step 4: Enter the activities necessary to enact the interventions
— Conduct further discussion with your groups regarding the activities involved in each intervention.
— Enter them on the MSAP template.
✤ Step 5: Enter the lead agency and relevant sector for each of the activities
✤ Step 6: Devise milestones/outputs for each activity
✤ Step 8: Establish indicators by which to measure the achievement of each objective
✤ Step 9: Enter the material you have gathered in Form 4.6 into the Implementation Plan section on the MSAP template
Click here to back to main text
ACTION 13: Create a costing sheet for the implementation of the MSAP
✤ Step 1: Enter the interventions and activities you have identified on a spreadsheet
✤ Step 2: Estimate the cost of delivering health services at national, provincial district level
— Take into account existing networks and the capacity of the available health facilities, including the human resources profile.
✤ Step 3: Enter the totals per year in the MSAP template
Click here to back to main text
ACTION 14: Develop implementation strategies
✤ Step 1: Form a stakeholder group to develop implementation strategies
✤ Step 2: Review the MSAP Framework
— Review the MSAP Framework to ensure that the implementation strategies you develop will align with the goal, NCD targets, strategic action areas and strategic objectives.
✤ Step 3: Develop strategies for implementing the MSAP
Use the following questions as a guide for deciding on the most beneficial strategies for your implementation team to implement the MSAP for NCDs:
— What resources and assets are there that can be used to help achieve the goal? How can they be used most effectively?
— What obstacles or resistance are there to achieving the goal? How can you minimize or get around them?
— What are potential agents of change willing to do to serve the mission?
— What strategies will develop policies or investment in order to meet the implementation of the MSAP?
— What strategies will strengthen capacity of the health facilities, in particular at the level of primary health care (PHC), to deliver the health service for NCD prevention and control?
— What strategies will strengthen the capacity of health workers, in particular at PHC level, to provide health counselling and service for patients?
— What technical guidelines or protocols need to be developed to provide guidance on early detection and appropriate treatment of main NCDs?
— What strategies will improve multisectoral action for NCD prevention and control?
✤ Step 4: Enter the implementation strategies you develop into the MSAP template
CHECKLIST
Use the Checklist available here to make sure you have completed all the necessary steps before moving on to the next module.
Noncommunicable diseases (NCDs) are the leading cause of death globally, killing more people each year than all other causes combined. Contrary to common perceptions, available data show that nearly 80% of NCD-related deaths occur in low- and middle-income countries. Moreover, recent decades have witnessed a steady increase in such deaths, with vulnerable population groups often worst affected, and yet many of the dire human and social consequences could be prevented by implementing cost-effective and feasible interventions.
The Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases (2011) (1) recognizes the scale of the NCD crisis and the urgent need for action. The Global action plan for the prevention and control of NCDs 2013–2020 (2) , recently extended to 2030, provides a vision and a road map to scale up action for the prevention and control of NCDs.
The global epidemic of NCDs is widely acknowledged as a major challenge to development in the 21st century and is a significant threat to achieving the United Nations Sustainable Development Goals. In addition, globally, the main NCDs represent the greatest cause of death in people aged under 70 years, imposing years of disability on those affected and their families. The Global status report on noncommunicable diseases 2014 (3) highlights the need to intensify national multisectoral action to meet the global targets that governments have agreed upon and to protect people from cardiovascular diseases, cancers, diabetes and chronic respiratory diseases.
Countries, including some that are low-income, are showing that it is feasible to make progress and reduce premature deaths from NCDs. But that progress, particularly in low- and middle-income countries, is insufficient and uneven. The global status report of 2014 reveals a distressing gap in our ability to achieve Sustainable Development Goal target 3.4 of reducing, by one third, premature deaths from NCDs by 2030, and outlines the disparities in progress on preventing NCDs worldwide.
This toolkit is a “how to” guide for developing, implementing and evaluating a multisectoral action plan for prevention and control of NCDs. It is targeted at policy-makers, planners and programme managers, and is intended to help countries, provinces and cities meet the requirements for achieving global and national NCD targets and the Sustainable Development Goals.
The toolkit takes the user through a series of actions related to the development of a multisectoral action plan (“MSAP development actions”), and provides forms and a template framework for users to complete as they undertake these actions.
Developing a multisectoral action plan involves establishing health needs and engaging relevant stakeholders before determining the actions to take, identifying and prioritizing interventions, deciding on ways to address. NCDs while establishing support and resources for prevention and control, and evaluating progress in implementing the plan.
Using the toolkit is an inclusive and participatory process that involves engaging relevant stakeholders before determining the actions to take. The toolkit focuses on the main NCDs and wider determinants of health and aims to reduce the premature mortality from NCDs and the negative impacts of these determinants on health and health inequalities.
This work entails an array of competencies, such as situation analysis, advocacy, planning, mobilizing, implementing interventions and evaluating them, and disseminating the results of the evaluation. Users can refer to programme theory and logic modelling to guide the development of their action plan. The structure of the toolkit is set out in Fig. 5.1.
Fig. 5.1 Structure of the toolkit for developing a multisectoral action plan for noncommunicable diseases
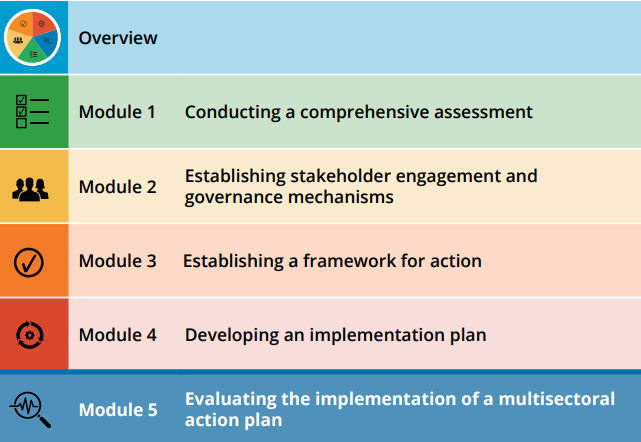
This module provides detailed guidance on how to evaluate implementation of a multisectoral action plan. Evaluation should be done on a regular basis to discern if the plan is reaching its goal and achieving its outcomes, and if it is doing so in an efficient manner. A well-designed evaluation can serve to motivate stakeholders and enhance national and local advocacy efforts. How this is to be achieved is an important final part of the toolkit.
Key stakeholders must be involved in the planning, implementation, monitoring and evaluation of NCD plans and programmes. Within a ministry of health there will be different types of stakeholders, such as programme managers and senior managers in departments of prevention, health promotion, and hospital and health services. Other stakeholders may come from ministries for transport, economics, agriculture, and education, funding partners, nongovernmental organizations, civil society and community members.
It is critical to ensure that there are clear and accurate descriptions of the policies, plans and programmes, so that all interventions, activities and desired outcomes are clearly understood by all involved in their evaluation.
The reasons for a particular monitoring and evaluation activity should be clearly defined at the outset. It is also important to state who the intended users are of the information that will result, and when they will require the information. If the purpose is not clear, there is a risk that the evaluation activity will focus on the wrong issues, draw the wrong conclusions and provide recommendations that will not be useful to the intended users.
A simple stakeholder assessment such as that outlined in Module 2 can help the evaluation team identify key individuals or groups to engage in the evaluation of the multisectoral action plan.
Stakeholders can make meaningful contributions during all phases of the evaluation, including evaluation planning, implementation, and the sharing and use of findings. Based on evaluation needs and stakeholders’ skills and interests, members of the evaluation stakeholder group can be engaged as:
— external reviewers of the evaluation plan and methods
— members of the evaluation advisory committee
— data sources (i.e. participants in evaluation interviews and surveys)
— data collectors
— data analysts
— interpreters of findings
— writers (e.g. of final evaluation reports, manuscripts, briefs) and presentation developers
— presenters or advocates who share findings with community partners and policy-makers.
It is not necessary for all stakeholders to participate in all phases of the evaluation. Some may contribute only to evaluation planning, while the participation of others may be limited to providing implementation support or sharing the evaluation findings.
This section will take you through the process of designing your evaluation framework and methodology. By the end of the section you will be in a position to complete the evaluation section of the MSAP template (which can be downloaded here) .
The focus of any evaluation will be a reflection of whether the plan is at the planning stage, being implemented, or at the stage of maintaining its outcomes and achievements. An evaluation at the planning stage will have a very different focus from one of a plan that has been in existence for several years.
For an evaluation during the planning stage, the following questions need to be addressed:
— What are the strategic direction, vision, strategies and key components of the plan?
— What is the plan's target population?
— How does the plan reach them?
— What is the coverage of the interventions?
— How much will it cost?
An evaluation that included outcomes would make little sense at the planning stage. Conversely, an evaluation of the plan during the maintenance stage would need to include some measurement of progress on outputs and outcomes.
Evaluation can focus on the implementation process and/or the effectiveness of its outcomes, but often both will be required. It will depend on the stage of implementation of the plan. This module provides guidance on both, examples of which are provided in Table 5.1.
Process evaluation and outcome evaluation
Process evaluations document the process of implementation. Process evaluations help stakeholders see how an MSAP outcome or impact was achieved. Process evaluations cover all aspects of the process to deliver a plan and are useful for:
— tracking the reach of the plan;
— tracking the level of implementation of all aspects of the plan; and
— identifying potential or emerging problems – whether the plan has been delivered as planned and whether modifications to the plan need to be made.
The focus of a process evaluation is the:
— types and quantities of services delivered;
— beneficiaries of those services;
— resources used to deliver the services;
— practical problems encountered; and
— ways in which such problems were resolved.
Outcome evaluations assess the effectiveness of the plan in producing change. Outcome evaluations focus on difficult questions that address what happened to participants of the plan and how much of a difference the plan made to them. Outcome evaluations are undertaken when it is important to know whether and how well the objectives were met.
Table 5.1 Type of evaluation: process or outcome
A number of evaluation questions may arise over the life of a multisectoral action plan that might reasonably be asked at any point in time. Addressing the questions about plan effectiveness means putting resources into documenting and measuring the implementation of the plan and its success in achieving intended outcomes and, in turn, using such information to be accountable to all stakeholders.
Evaluation questions should reflect the purpose of the evaluation and the priorities and needs of the stakeholders. They should help focus the evaluation and provide information about the plan’s components/activities. Evaluation teams needs to classify the questions as overall progress, process, or outcome evaluation questions.
Overall progress evaluation questions
Overall progress evaluation questions are concerned with how well the plan is being implemented in general, and therefore tend to be fairly broad, as can be seen in Table 5.2.
Table 5.2 Example questions for the review of implementation progress
| In what context is the a multisectoral action plan operating? |
|---|
| Is the plan accomplishing its intended results? |
| What were the key achievements? |
| Which factors have supported or challenged the implementation? |
| Which parts of the plan are working? Which parts are not working? Do resources need to be refocused? |
| Has equity in health improved? |
| Are there any international collaborative actions for NCD prevention and control? |
| Have plan participants (staff, community organisations, community members) been satisfied with the plan? |
| Has the uptake of the plan varied by socio-economic position or rural/metropolitan location? |
| How effective were the contracting and subcontracting arrangements that were established to support plan implementation and evaluation? |
Process evaluation questions
Process evaluation questions are primarily concerned with the actual delivery of the plan – its governance and implementation.
Process evaluation questions should incorporate key process components of the logic model (inputs, activities, and outputs). Tables 5.3 and 5.4 below provide examples of process evaluation questions.
Table 5.3 Example process evaluation questions related to governance
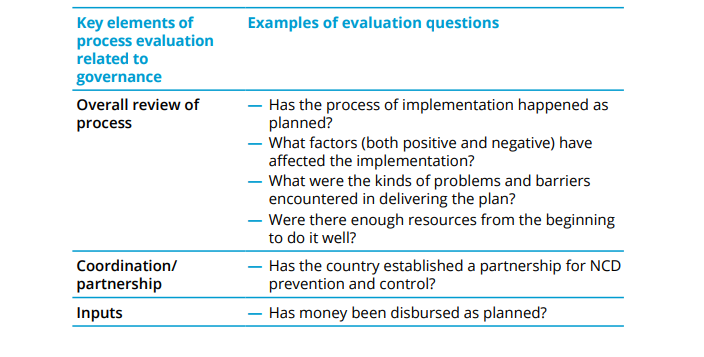
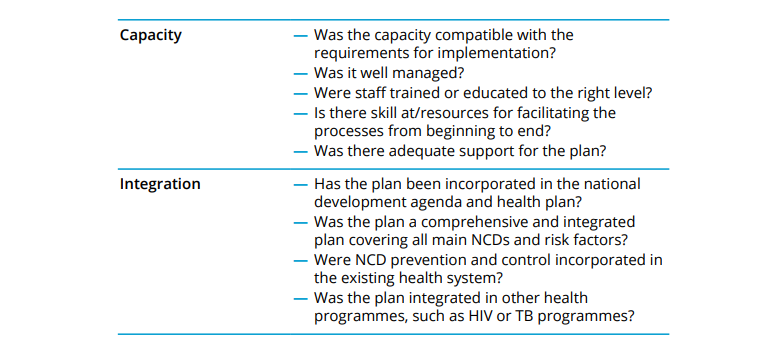
Table 5.4 Example questions related to other strategic areas of NCD prevention and control
Outcome questions
Outcome evaluation questions are concerned with the effects of the delivery and operations of the multisectoral action plan on the target population(s). They should address key outcome components from the logic model discussed in the Overview. Depending on whether they are short-, intermediate- or long-term outcomes, they can be reviewed annually, in the medium-term, or during the final review. Table 5.5 presents example questions for outcome evaluations of a plan.
Table 5.5 Example questions for outcome evaluation of NCD prevention plan and programmes
After working with stakeholders to identify focus areas for the evaluation and the framing of the evaluation questions, the evaluation team should identify indicators for each of the evaluation questions.
Indicators should be visible, measurable signs of performance. Note that an evaluation question may have more than one indicator. Most multisectoral action plans will not require an extensive list of indicators, and preference should be given to quality rather than quantity. Table 5.6 presents examples of questions and indicators for an evaluation question related to partnerships.
Table 5.6 Example questions and indicators for evaluation of a multisectoral action plan intervention
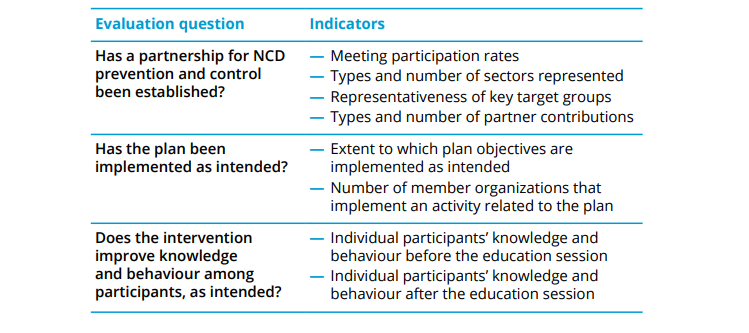
MSAP DEVELOPMENT ACTION 15: Work with stakeholders to frame the evaluation
Establishing a budget
You will need to establish a source of funding and a budget for the evaluation. This will have a major impact on who conducts the evaluation and the way in which it is managed.
Establishing an evaluation team
It will be necessary to establish a team to conduct and manage the evaluation, but before building the team it is important to consider what evaluation skills or approaches are needed to successfully conduct this evaluation.
You may prefer the evaluation to be managed from within your organisation, or decide that it would be advisable and feasible to bring in outside experts to conduct the evaluation and report its findings.
Working out a timeline
If the evaluation is being done within the organisation a timeline will need to be worked out that incorporates the following tasks:
— planning and administration
— training of data collectors
— data collection, analysis, and interpretation
— information dissemination.
Once this has been mapped on to a timeline, check for any foreseeable bottlenecks or sequencing issues.
When gathering data for the evaluation, you will need to consider what methods are appropriate for the data, and for obtaining answers to the evaluation questions posed.
The following points will need to be considered:
— Will new data be collected to answer the evaluation questions and/or will secondary data be used? Can you use data from the performance measurement system?
— What methods will be used to collect or acquire the data?
— How will data collection instruments be identified or created?
— How will instruments for readability, reliability, validity, and cultural appropriateness be tested?
— How will the quality and utility of existing data be determined?
Table 5.7 provides examples of the main methods for data collection and potential data sources for use in evaluation.
Table 5.7 Sample of data collection methods and potential data sources
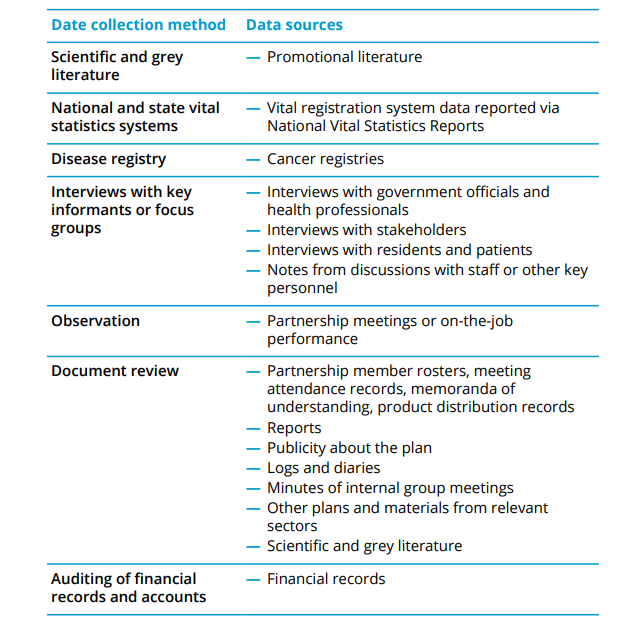
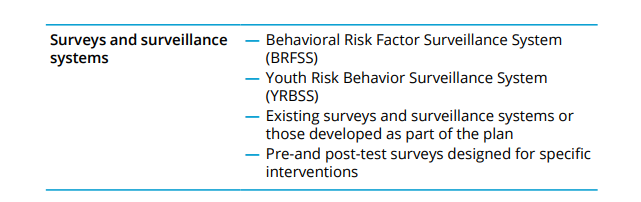
Table 5.8 provides example indicators, an example data source and an example data collection method for a partnership evaluation question.
Table 5.8: Example indicators, data source and data collection method for partnership evaluation question
MSAP DEVELOPMENT ACTION 16: Work with stakeholders to plan data collection
After designing an evaluation and collecting the data, the information must be described, analysed, and interpreted, so a judgment can be made about the meaning of the findings in the context of the multisectoral action plan. There are many methods of evaluation and it is not possible for a practical guide to adequately explain them all. In this section we will look at just some of the basic techniques for managing and analysing data.
Data management is the process of ensuring the data collected is a valuable resource for the prevention and control of NCDs. Capacity to conduct the following activities is essential:
— data storage
— data quality assurance
— data processing and compilation.
Once data are collected, they need to be systematically and carefully analysed. In some cases, data can be tabulated manually, in others computer programmes can help with the processing and summarizing of both quantitative and qualitative data.
The importance of valuing and seeking multiple perspectives comes into play during this phase of the evaluation. Quantitative data analysis requires interpretation of the results and seeing if they make sense, given the project’s contextual factors – something the staff involved will know better than most.
Project staff and the evaluation team should work together and ask:
— Do these results make sense?
— What are some possible explanations for findings that are surprising?
— What decisions were made about categories and indicators of success? Have we missed other indicators?
— What decisions were made about categories and indicators of success? Have we missed other indicators?
— How might what we choose to collect and analyse be distorting the programme/initiative?
— And, most importantly, how will the numbers and results help us decide what actions will improve the programme?
Qualitative data includes information gathered from interviews, observations, written documents, journals, or even open-ended survey questions. Information gathered from interviews and observations is often recorded in lengthy narratives or field notes. In some cases, interviews are tape-recorded and then transcribed.
Some of these accounts are useful and can stand alone – providing important information about how the plan is working. In most cases, however, it is valuable to analyse your qualitative data in more systematic ways.
The quantitative and qualitative data gathered can be used to answer the evaluation questions posed by the stakeholders in Action 15, and to make an assessment of the success with which each aspect of the plan being evaluated has been implemented.
Achievements in reducing major risk factors, strengthening surveillance, building capacity, or establishing research networks should all be noted. Where the implementation process has not gone smoothly, or the outcomes have been lower than expected, it is important to work out what factors have contributed to this.
Recommendations may need to be made about future action, such as capacity building, the raising of additional funding, and further engagement with stakeholders.
MSAP DEVELOPMENT ACTION 17:Liaise with project staff over analysis of results
Whatever the strategy you develop for disseminating the findings of your evaluation, it will be helpful to draft and finalize a full-findings report with evaluation stakeholders, from which information can be extracted to develop more concise results documents tailored to specific audiences.
In general, a detailed evaluation report should include:
— executive summary
— evaluation background and purpose
— acknowledgement of who commissioned and conducted the evaluation
— description of how the evaluation was conducted, what methods were employed, and in what timeframe
— evaluation results and limitations
— summary of the findings and recommendations
— annexes containing relevant information about working procedures and more detailed information about the data (such as tables).
A more detailed outline can be found in Annex B.
This section offers guidance about the presentation and communication of evaluation results. Disseminating evaluation results to internal and external stakeholders and other interested parties can fulfil many objectives. These may include demonstrating the plan’s relevance, improving working practices, accounting to funding and regulatory bodies, informing local communities and gaining support for current and future plans. This section will help the evaluation team do the following:
— identify the key components of an evaluation report;
— determine with whom to share the evaluation results and when and how to share these findings;
— describe the steps that programme managers will take to ensure that evaluation findings will be used to inform plan improvement efforts; and
— apply these skills by using the guides provided in this section.
You will need to consider who the main audiences are for the report on your findings – which will depend on whether the report is on the progress of the implementation or on the outcomes of the plan – and the purpose of the communication. This will lead you to consider the most appropriate method of communication and the most suitable “messenger”.
The timing of the communication might also need to be considered. There may be a pre-arranged event that serves as a deadline for the completion of the full evaluation report.
Your detailed evaluation report will form the bedrock of other formats for summarizing and reporting evaluation results, including the following:
— an executive summary of the evaluation report
— a slide presentation
— a briefing
— a brochure
— a website
— an article in a newsletter
— a radio or television spot.
Many of these options can be presented in electronic and hardcopy formats.
The evaluation team should take a practical and creative approach to dissemination – the process of communicating evaluation methods and findings to relevant audiences in a timely, unbiased and consistent manner. Staff should share ideas early on in the evaluation process about what steps they will take to ensure evaluation findings are used to inform programme improvement and expansion efforts.
Planning for the dissemination and utilization of evaluation findings builds on previous efforts to engage stakeholders, develop the multisectoral action plan and focus the evaluation design. Having a clear picture of the plan, stakeholder interests, and evaluation priorities and activities will help the evaluation team identify appropriate strategies for sharing and utilizing the findings.
Regardless of how communications are constructed, the goal for dissemination is to achieve full disclosure and impartial reporting. The tips provided in this section will help the evaluation team develop and carry out a dissemination strategy that best suits the plan.
Above all, the presentation of the evaluation should always be linked to the initial aims and objectives, as well as to the target audiences. There is a variety of ways of presenting results, but a detailed written report forms a useful resource of information for use in other formats, such as oral presentations, press releases, and media communication.
The knowledge, needs and interests of the target audience(s) will determine the information to be included in the report. Depending on the target audience, the level and scope of content can vary even when addressing the same issues. For some audiences it may be necessary to outline the background and the reach of the plan and the objectives of the intervention(s). For those involved in the project, this may not be necessary. However, the objectives of the evaluation should always be clearly set out.
MSAP DEVELOPMENT ACTION 19: Disseminate the findings of the evaluation
It is helpful to strategize with stakeholders early in the evaluation process to ensure that findings are used to improve the plan. That way, as important evaluation findings are produced, the evaluation team can work with programme staff to apply them in a timely and efficient manner.
Several practical steps can be taken to help ensure evaluation findings are used to improve the MSAP framework and implementation. These include, but are not limited to, the following:
— Use regularly scheduled meetings with evaluation stakeholders as a forum for sharing evaluation findings in real time, and developing recommendations for programme improvement based on these evaluation findings.
— Encourage programme directors and/or programme coordinators to include a review of evaluation findings and recommendations in regularly scheduled staff meetings.
— If resources allow, identify a programme staff member to coordinate, document, and monitor the efforts that programme staff and partners are making to implement improvement recommendations.
MSAP DEVELOPMENT ACTION 20:Utilize the results of the evaluation
Key Messages
— Key stakeholders should be involved in the evaluation of the implementation of a multisectoral action plan.
— The reason for an evaluation and its intended users should be defined at the outset.
— The focus of an evaluation will be different, depending on what stage the plan is at.
— Process evaluations document the implementation, and help show how outcomes and impact are being achieved.
— Outcome evaluations assess the effectiveness of the plan in changing the circumstances of those the plan is designed to benefit.
— Evaluation questions should reflect the purpose of the evaluation and the priorities and needs of the stakeholders.
— Progress evaluation questions are concerned with how well the plan is being implemented in general.
— Process evaluation questions are primarily concerned with the actual delivery of the plan – its governance and implementation.
— Outcome evaluation questions are concerned with the effects of the delivery and operations of the plan on the target population.
— The evaluation will need a source of funding and a budget.
— The evaluation will need a team to manage it.
— Methods for collecting data need to be appropriate to the data and for obtaining answers to the evaluation questions posed.
— Both quantitative and qualitative data can be used to answer the evaluation questions posed by stakeholders.
— Recommendations may need to be made about future action, such as capacity building, the raising of additional funding, and further engagement with stakeholders.
— A full-findings report will be a helpful resource from which to extract a summary and key findings for dissemination.
— Disseminating evaluation results to internal and external stakeholders and other interested parties can fulfil a range of objectives.
— The main audience for your findings will affect the method and timing of the communication.
— It is helpful to strategize with stakeholders early in the evaluation process to ensure that findings are used to improve the plan.
- CDC. Behavioral Risk Factor Surveillance System (BRFSS) [online database] Atlanta (GA) : Centers for Disease Control (https://www.cdc.gov/brfss/index.html).
- CDC. National Vital Statistics Reports (NVSR) [online database]. Atlanta (GA): Centers for Disease Control (https://www.cdc.gov/nchs/products/nvsr.htm).
- CDC. Youth Risk Behavior Surveillance System (YRBSS) [online database] Atlanta (GA): (https://www.cdc.gov/brfss/index.html).
- WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization (https://apps.who.int/iris/handle/10665/94384).
- WHO (2013). Resolution WHA66/10. Follow-up to the political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. In: Sixty-sixth World Health Assembly, Geneva, 20–27 March 2013. Resolutions and decisions, annexes. Geneva: World Health Organization:16–20 (WHA66/2013/REC/1; http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_R10-en.pdf).
- Political declaration of the high-level meeting of the General Assembly on the prevention and control of non-communicable diseases. New York: United Nations; 2011 (A/RES/66/2; ( https://digitallibrary.un.org/record/720106,accessed 1 November 2021).
- Global action plan for the prevention and control of NCDs 2013–2020. Geneva: World Health Organization; 2013 ( https://apps.who.int/iris/handle/10665/94384,accessed 1 November 2021).
- Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014 (http://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf?sequence=1, accessed 1 November 2021).
-
Citation
World Health Organization. (2022). Toolkit for developing a multisectoral action plan for noncommunicable diseases: module 5: evaluating the implementation of a multisectoral action plan. World Health Organization. https://apps.who.int/iris/handle/10665/353162. License: CC BY-NC-SA 3.0 IGO.
ISBN of Module 5 is -9789240043572 (electronic version)
9789240043589 (print version)
- Bamberger M, Rugh J, Mabry L (2006). Real world evaluation: working under budget, time, data, and political constraints. Thousand Oaks, CA: Sage Publications, Inc.
- CDC (2011). Introduction to program evaluation for public health programs: a self-study guide. Atlanta (GA): Centers for Disease Control and Prevention ( https://www.cdc.gov/evaluation/guide/index.htm ).
- Chen HT, Morosanu L, Powell-Threets K, Lian B, Turner N (2019). Assessment of the monitoring and evaluation system of a population-based program: theory- driven evaluation approach. Eval Program Plann. 77:101719. doi: 10.1016/j. evalprogplan.2019.101719.
- Evans R, Scourfield J, Murphy S (2015). Pragmatic, formative process evaluations of complex interventions and why we need more of them. J Epidemiol Community Health. 69(1):925-6.
- Funnell SC (2004). Developing and using a program theory matrix for program evaluation and performance monitoring. New Directions for Evaluation. 2000(87):91- 101.
- Gamble JA (2008). A developmental evaluation primer. Montreal: JW McConnell Foundation. Gauri SK, Das P (2017).
- Gauri SK, Das P (2017). A framework for performance evaluation and monitoring of public health program using composite performance index. Int J Quality Res. 11:817-33. doi: 10.18421/ijqr11.04-06.
- Gertler PJ, Martinez S, Premand P, Rawlings LB, Vermeersch, CMJ (2011). Impact evaluation in practice. Washington, DC: The International Bank for Reconstruction and Development/The World Bank (https://pdfs.semanticscholar.org/42c8/b526b2d095eeaae15335f98c1e6d7316fe2e.pdf).
- Guinea J, Sela E, Gomez-Nunez AJ, Mangwende T, Ambali A, Ngum N et al (2015). Impact oriented monitoring: a new methodology for monitoring and evaluation of international public health research projects. Research Evaluation. 24(2):131-45. doi: 10.1093/reseval/ rvu034.
- Issel LM. (2009). Health program planning and evaluation: A practical, systematic approach for community health (2nd ed). Sudbury, MA: Jones and Bartlett Publishers.
- Ivankova NV, Creswell JW, Stick S (2006). Using mixed methods sequential explanatory design: from 488 theory to practice. Field Methods. 18(1):3–20.
- Khandker SR, Koolwal GB, Samad HA (2010). Handbook on impact evaluation. Washington, DC: The International Bank for Reconstruction and Development/The World Bank (http://documents.worldbank.org/curated/en/650951468335456749/pdf/520990PUB0EPI1101Official0Use0Only1.pdf).
- Kusek JZ, Rist RC (2004). Ten steps to a results-based monitoring and evaluation system. Washington, DC: The International Bank for Reconstruction and Development/The World Bank (https://www.oecd.org/dac/peer-reviews/World%20bank%202004%2010_Steps_to_a_Results_Based_ME_System.pdf).
- Mackay K (2007). How to build M&E systems to support better government. Washington, DC: World Bank (https://openknowledge.worldbank.org/handle/10986/6851?show=full).
- Murphy MM, Unwin N, Samuels T, Hassell TA, Bishop L, Guell C (2019). Evaluating policy responses to noncommunicable diseases in seven Caribbean countries: challenges to addressing unhealthy diets and physical inactivity. Rev Panam Salud Pública. 42:e174.
- Nolte E, Knai C, Saltman RB, editors (2014). Assessing chronic disease management in European health systems: concepts and approaches. Copenhagen: WHO Regional Office for Europe (Observatory Studies Series 37; (http://www.euro.who.int/__data/assets/pdf_file/0009/270729/Assessing-chronic-disease-management-in-European-health-systems.pdf).
- Porteous NL, Sheldrick BJ, Stewart PJ (1997). Program evaluation tool kit: a blueprint for public health management. Ottawa: Ottawa-Carleton Health Department.
- Rogers P, Hacsi T, Petrosino A, Huebner T, editors (2000). Program theory in evaluation: challenges and opportunities. New Directions for Evaluation. 87:91-101. San Francisco, CA: Jossey-Bass Publishers.
- Saunders RP, Evans MH, Joshi P (2005). Developing a process-evaluation plan for assessing health promotion program implementation: A how-to guide. Health Promotion Practice, 6(2):134-147.
- Shao R, Feil C, Wild CK, Morschel K, Bonyani A, Smith R et al (2021). Assessing the characteristics of 110 low- and middle-income countries’ noncommunicable disease national action plans. Int J Noncommun Dis. 6(2):56-71.
- Taylor-Powell E (2008). Building capacity in evaluating outcomes: a teaching and facilitating resource for community-based programs and organizations. Madison, WI: University of Wisconsin-Extension, Cooperative Extension, Program Development and Evaluation (https://kmmhasan.files.wordpress.com/2016/06/bceoresource.pdf).
- United Nations Development Programme (2009). Handbook on planning, monitoring and evaluating for development results (http://web.undp.org/evaluation/handbook/documents/english/pme-handbook.pdf).
- United Nations Evaluation Group (2016). Norms and standards for evaluation. United Nations Evaluation Group (http://www.unevaluation.org/document/detail/1914).
- WHO Regional Office for Europe (1996). Handbook for process evaluation in noncommunicable disease prevention. Copenhagen (https://www.euro.who.int/document/E66338.pdf).
Click here to back to main text
ACTION 15: Work with stakeholders to frame the evaluation
✤ Step 1: Decide on what you want to evaluate
— Are you evaluating overall progress, process, or outcomes?
— Consider the context of the priorities and needs of the stakeholders.
✤ Step 2: Decide on which components/activities of the MSAP you should focus on
— Refer to Form 5.1 for potential areas for consideration.
✤ Step 3: Develop your evaluation questions and related indicators
Record them on Form 5.1
Click here to back to main text
ACTION 16: Work with stakeholders to plan data collection
✤ Step 1: Identify suitable data sources for the indicators framed in Action 15
— Record them on Form 5.2
✤ Step 2: For each data source, decide on a data collection method
— Record them on Form 5.2
Click here to back to main text
ACTION 17: Liaise with project staff over analysis of results
You may need to establish subgroups of stakeholders to work on individual evaluation questions, or groups of questions.
Use Form 5.3 to focus discussion.
✤ Step 1: Discuss the data collected and the conclusions that can be drawn from it
✤ Step 2: Make a collective judgement of the answers to the evaluation questions
— Fill in the first two columns of Form 5.3
✤ Step 3: Elaborate on your answers, focusing on strengths, gaps/ weaknesses, and recommendations
— Fill in the remaining columns of Form 5.3
Click here to back to main text
ACTION 18: Prepare an evaluation report
Annex B in this module provides a possible structure for the report.
Form 5.4 provides a checklist of characteristics to help you ensure that your report communicates successfully with your target audience.
Click here to back to main text
ACTION 19: Disseminate the findings of the evaluation
You may need to establish a core team of communication specialists for this action.
Form 5.5 can be used to record how to disseminate your findings.
✤ Step 1: Identify the target audiences or groups of stakeholders with whom the findings will be shared
✤ Step 2: Identify suitable formats and channels for sharing the findings
✤ Step 3: Discuss the timing, style, tone and message of the information products you will need to create
✤ Step 4: Gain approval at the appropriate level for your plans for dissemination
✤ Step 5: Enter the approved plan into the Evaluation section of the MSAP template
✤ Step 6: Disseminate the findings of the evaluation
Click here to back to main text
ACTION 20: Utilize the results of the evaluation
✤ Step 1: Work with stakeholders of the MSAP to establish ways in which the recommendations from the evaluation can be shared with them and with team members
✤ Step 2: Identify a team member to be responsible for recording actions taken to address and implement the recommendations
— Provide them with Form 5.6 on which they can record efforts made to implement the recommendations for improvement (date, department, contact name, recommendation, action).
✤ Step 3: Record the actions in the MSAP template
CHECKLIST
Use the Checklist available here to make sure you have completed all the necessary steps.
The epidemic of NCDs is being driven by powerful forces, including demographic ageing, rapid unplanned urbanization, and the globalization of unhealthy lifestyles. NCDs and their risk factors are unevenly distributed within populations, and these inequalities need to be considered to ensure an effective mix of policy solutions is selected. Population and health indicators Health indicators are quantifiable characteristics of a population. These include, but are not limited to, population growth, crude birth rates, age adjusted death rates, maternal mortality ratios, female/male populations and infant mortality rates. Such basic information should be included when assessing the health status of a population.
Economic and health indicators Economic and health expenditure indicators include, but are not limited to, gross national income (GNI), inflation rate and health expenditure.
Social determinants of health The Social determinants of health are the circumstances in which people are born, grow, live, work and age, and the systems put in place to deal with illness. These circumstances are in turn shaped by a wide set of forces that include economics, social policies, and politics. Better health contributes to increased well-being, education, social cohesion, environmental protection, increased productivity and economic development. A circle is thus possible whereby improvements in health and its determinants feed back into each other, providing mutual benefits.
NCDs cannot be addressed effectively without action on social determinants of health. For example, local transport and housing policies are needed; national fiscal, environmental, education and social policies; and global financial, trade and agricultural policies. Understanding and modifying the social determinants of NCDs are crucial to addressing inequalities in NCDs and in health, between different social groups.
Social determinants need to be routinely monitored and factored into policy-making in order to evaluate the impact of policies and change course when necessary.
WHO Social determinants of health
WHO Health Accounts
WHO Commission on social determinants of health (2008). Closing the gap in a generation: health equity through action on the social determinants of health
WHO (2010). Equity, social determinants and public health programmes
WHO (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–20
WHO Global Health Estimates (GHE)
WHO Global Health Observatory (GHO) data
The United Nations (2011). UN Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases